Research Article - Clinical Schizophrenia & Related Psychoses ( 2021) Volume 0, Issue 0
2M.Sc., Department of Basic Studies, Family Research Institute, Shahid Beheshti University, Tehran, Iran
3Department of Medicine, Iran University of Medical Sciences, Tehran, Iran
4Department of Psychiatry Faculty of Medicine, Hormozgan, University of Medical Sciences, Bandar Abbas, Iran
Seyyed Hamzeh Seddiq, Department of Psychiatry Faculty of Medicine, Hormozgan, University of Medical Sciences, Bandar Abbas, Iran, Email: seddigh@gmail.com
Received: 16-Dec-2021 Accepted Date: Dec 30, 2021 ; Published: 06-Jan-2022
Abstract
Background and aim: One of the effects of exposure to COVID-19 is adverse psychological and mental health, and considering that people with Autism Spectrum Disorder (ASD) have a previous background in terms of mental health deficits; therefore, the study of the COVID-19 epidemic effect on the psychological reactions of individuals with ASD is of great importance, which is the main purpose of this study.
Materials and methods: For this purpose, all studies related to the subject from 2020-2021 by systematic search in internationally available databases including Web of Science, Science Direct, Scopus, PubMed, Google Scholar, and other databases were reviewed. Finally, 21 completely relevant studies were selected to extract the considering results.
Results: The results showed that caregivers and nurses of children with autism reported more anxiety during quarantine than children without autism. The results showed that the symptoms of depression and anxiety in response to this epidemic increased for both non-autism and autism groups. However, the incidence of these symptoms was higher for individuals with ASD. In addition, individuals with ASD showed greater concern about their pets, work, medication and food, and safety/security. In general, the results of this study showed that the increase in social isolation related to the epidemic had a severe and destructive effect on the mental health and mental well-being of autistic individuals. In addition, the COVID-19 epidemic increased stress and anxiety in parents of individuals with ASD.
Conclusion: According to the study, it can be concluded that ASD patients were more stressed and more anxious before the epidemic than normal people. Furthermore, this epidemic has a higher impact on individuals' mental health with ASD than normal people. Therefore, to maintain the mental health of autistic individuals during the COVID-19 outbreak, it is necessary to provide appropriate educational programs to reduce the psychological burden of this epidemic. In addition, health officials must provide more services and counselling for ASD individuals in this period of urgency.
Keywords
Autism spectrum disorder • COVID-19 • Psychological impact • Social isolation • Mental health
Introduction
On Jan 30, 2020, the World Health Organization (WHO) announced the emergence of a new coronavirus and declared a public health emergency. On Mar 11, 2020, the WHO formally named the Coronavirus (COVID-19). The disease has been the largest outbreak since the acute outbreak of Severe Acute Respiratory Syndrome (SARS) in 2003. It has rapidly affected governments and public health systems with the possibility of severe respiratory illness [1].
There has been a worldwide public health effort to prevent coronavirus transmission after its global spread. However, the campaign encouraged people on a large scale to distance themselves, leading to social isolation. Therefore, it can be said that creating social distance to prevent the spread of corona has a great impact on the way people live and socialize daily [2]. In addition, the epidemic itself and the resulting behaviours and daily activities have profoundly affected mental health [3,4]. Previous studies have been performed in prior epidemics such as equine influenza [5], SARS [6,7], H1N1 [8], as well as the current COVID-19 epidemic [9-15], that evidence of such epidemics harmed people's mental health.
It is important to note that although the COVID-19 epidemic affects the whole population, the adverse mental health effects of this epidemic may not be evenly distributed to all sections of society. For example, people with Autism Spectrum Disorder (ASD) may be considered one of the most vulnerable groups in this epidemic, likely affecting them more than other sections of society [16].
Autism is a common neurodevelopmental disorder with a global prevalence estimated at 0.62% or more [17]. However, the impact of this epidemic may be more substantial for people with ASD for two main reasons: The first reason is that ASD itself is associated with an increased risk of mental health problems such as mood disorders and anxiety [18,19]. The second reason is that ASD is characterized by two main aspects of the symptoms directly affected by the epidemic. On the one hand, individuals with ASD experience problems in social and communication interactions (such as problems starting or responding to social interactions, adjusting their behaviour to different social situations, and developing and maintaining relationships). On the other hand, people with autism show limited and repetitive behaviours, interests, and activities. The second domain insists on uniformity and strict procedures, which sometimes leads to severe distress in response to small changes [20].
These two main aspects of autism symptoms are directly affected by the COVID-19 epidemic. It affects both the social interactions of ASD patients and leads to extensive and continuous changes in their daily lives. Therefore, it can be said that people with autism may uniquely experience the COVID-19 epidemic. Due to this fact, based on previous studies, it has been reported that adults with ASD have more difficulty coping with stressful events than neurotypicals [21,22]. Since, in general, the level of anxiety and depression in the autistic population is high [18,19], further research is needed to determine the epidemic's impact on the mental health of people with autism. Therefore, this study aimed to investigate the effects of the COVID-19 epidemic on psychological outcomes in individuals with autism by a narrative review study.
Materials and Methods
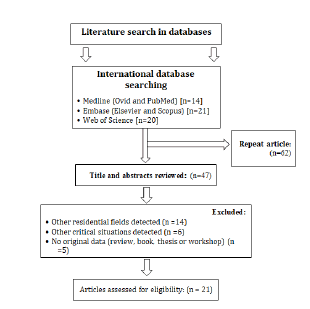
To review and extract required results from published articles and reports related to the considered subject, a systematic search of internationally available databases, including Web of Science, Science Direct, Scopus, PubMed, and Google Scholar, was done from 2020 to 2021. Systematic review using the Mesh terms "Mental Health", "COVID-19", "ASD", "Autistic", "Patients", "Children", "Adults" and "Autistic spectrum disorder", "Social isolation", "Anxiety", "Stress", "Pandemic", "Depression", "Distress" and "Mental wellbeing" were performed. For other databases, the same mesh terms were used similarly. The references were thoroughly reviewed to ensure that no articles were missed from the study (Reference Checking). In addition, the citations from the research were also checked (Citation Tracing) to ensure that the search was complete. Based on Figure 1, the literature review, especially articles, was performed based on the PRISMA guideline [22]. In addition, unofficial reports, articles in a letter to editor format, and unpublished articles and content posted on Internet sites were removed from the list of downloaded files. Finally, the results of 21 published articles were reviewed for the present review study.
Results and Discussion
The need for further research on COVID-19 and autism and to study the impact of people's concerns with autism during the COVID-19 epidemic is essential [23-30]. In the study of Asbury, et al. parents of school children with special educational needs and children with disabilities were interviewed to describe the impact of the COVID-19 epidemic on their child's mental health. In this study, most of the sample size was the parents of a child with autism (82%). Based on the results of this study, it was reported that these children developed anxiety/worry during this epidemic [25].
In Amorim, et al. study, caregivers and nurses of children with autism reported more anxiety during quarantine than children without autism. In addition, most caregivers in the autism group said that quarantine hurt emotion management in their children. In contrast, most parents without autism reported no or even a positive effect of quarantine on their children's emotional management [28].
According to Mutluer, et al. the COVID-19 epidemic has increased behavioural problems in children with ASD since the onset [30]. According to Colizzi, et al. pre-existing behavioural problems predict a higher risk for more severe and recurrent behavioural issues during the epidemic [31]. Based on the study of Ameis, et al. it was reported that the potential negative impact of the COVID-19 epidemic on changes in daily life routines as well as restrictions on regular services on children with ASD is quite evident [24]. A study by White, et al. which surveyed caregivers of children with ASD, reported that the COVID-19 epidemic disrupted services and treatments for individuals with autism. The National Autism Association said that 9 out of 10 people with autism are concerned about their mental health [26].
In the study of Oomen, et al. on the psychological impact of the COVID-19 epidemic on 1,044 adults with ASD in three European countries, including the United Kingdom, Belgium, and the Netherlands, the results showed that the symptoms of depression and anxiety in response to the epidemic for both the non-autism and autism groups have increased. However, the incidence of these symptoms was higher for adults with ASD. In addition, adults with ASD showed greater concern about their pets, work, food and medicine, and safety/security. People with ASD felt that although they were relieved by social stress, they experienced the loss of social contact as a problematic issue. Adults with ASD also experienced more stress due to losing their routine programs.
Based on the results of a study by Oomen, et al., In addition to the negative effects of this epidemic on ASD patients mentioned above, the positive impact of this epidemic was to make pleasant changes in adults with autism due to increased correlation and reduced sensory and social burden. Based on the study results, adults with ASD often reported cancelling guidance due to this epidemic and expressed their desire to receive more information and specific recommendations for autism [20]. In addition, increased concern about their pets in adults with autism in a study by Oomen, et al. was interesting because a previous pre-epidemic study by Dachez and Ndobo showed that some adults with autism seek to support pets as a coping strategy [32].
In a qualitative study conducted by Pellicano, et al. 144 individuals, including adults with autism (44 people), parents of children with autism (84 people) and parents of autism, and young people with autism (16 people), were interviewed about the impact of the COVID-19 epidemic on social isolation and mental health, as well as their families. This study showed that increasing social isolation and the epidemic had a severe and destructive effect on the mental health and mental well-being of autistic individuals. People with ASD complained bitterly about the loss of friends and social networking due to the epidemic. In addition, participants in this study were sometimes extremely dissatisfied due to replacing one-on-one communication in health services with online/telephone communication [1]. Other similar studies include Adams, et al. [33], Amorim, et al. [28], Asbury, et al. [25], Bal, et al. [34], Oakley, et al. [35] and White, et al. [26] have been reported that the quarantine created by the COVID-19 epidemic, has caused various psychological distress to autistic children and their parents.
The findings from the above studies show that this distress may partly be due to a lack of social interaction. According to these studies, the inability to enjoy social interactions is challenging for autistic people, even if social media and other digital technologies reduce some adverse effects. Moreover, some autistic individuals in COVID-19 appear to rapidly become much more isolated, as has been commonly documented in the general community [36,37].
It is important to note that the adverse effects of loneliness and isolation on mental and physical health in regular times have been well established [38]. However, the findings of Pellicano, et al. show that the experience of autistic individuals during the COVID-19 epidemic (for adults, children, adolescents, and parents) was not psychologically different from the experience of non-autistic individuals. This has also been reported in Loades, et al. [39]. However, in the study by Hedley, et al. the potential effects of loneliness on depression and self-harm thoughts have been reported only in autistic adults [40]. Further research is therefore needed to identify specific ways in which autistic individuals can enhance reciprocal supportive social communication based on their circumstances in the future.
Another issue related to the COVID-19 epidemic is the negative impact on parents of children with ASD. Parents of children with ASD experience significant amounts of stress and impaired emotional well-being. As a result, parents of children with ASD may experience stress and anxiety due to the COVID-19 outbreak's adverse effects on their children's programs. A study by Ersoy, et al. aimed to compare the impact of health anxiety on the dispositional hope and the psychological well-being of mothers with autistic children and mothers with normal children in the Covid-19 epidemic in Turkey. The participants in this study are 126 mothers (60 mothers with autistic children and 66 mothers with normal children) living in Istanbul. According to this study, mothers of autistic children were more likely to experience anxiety problems than mothers of non-autistic children. In addition, according to the results of this study, mothers with autistic children were more likely to have higher levels of general anxiety and anxiety about chronic diseases than mothers with normal children. In addition, they were more likely to have lower levels of hope and mental well-being [41].
In addition, the Alhuzimi study aimed to investigate the stress and emotional well-being of parents of children with ASD in Saudi Arabia during the COVID-19 epidemic. This study selected 150 parents of children with ASD from different parts of Saudi Arabia using an online poll. The study results showed that the demographic status of children with ASD (especially age, sex, and severity of symptoms) significantly affects parental stress and emotional well-being. In addition, parents were affected by changes in the severity of ASD behaviours in children with ASD. Finally, it was found that parental stress harms parents' emotional well-being [42].
Conclusion
Based on the results of this review study, it is clear that the psychological burden of the COVID-19 epidemic on people with autism is quite evident and prominent. Therefore, these people feel the need for more accessible and affordable health care support. The results showed that the symptoms of depression and anxiety in response to this epidemic increased for both non-autism and autism groups. However, the incidence of these symptoms was higher for people with ASD. In addition, people with ASD showed greater concern about their pets, work, medication and food, and safety/security. The present study's findings show that supporting autistic individuals is vital for maintaining direct social contact during and after the epidemic. Furthermore, the results of this study showed that parental stress and the emotional well-being of parents of children with ASD were adversely affected by the COVID-19 epidemic. Based on the findings of the present study, providing various educational programs to help children with ASD as well as their parents (to modify the characteristic behaviours of children with ASD such as the ability to maintain a schedule, and prevent aggressive behaviours and also to reduce the psychological burden of type of epidemic) is recommended.
References
- Erdenen F, CS, Karşidağ and Altunoğlu E. “Evaluation of Disability, Anxiety and Depression in Hemodialysis Patients.” Nobel Med 6 (2010): 39-44.
- Abbas, Amjed H, Muna Abdulridha Rasheed, Hayder Abdul-Amir Al-Hindy, Mazin J Mousa and Hadeel Abd Ameir Al-Shalah. “The Role of Serum IL-1β in Combination with Fractional Exhaled Nitric Oxide in the Diagnosis of Adult Bronchial Asthma.” Neuro Quantology 19 (2021): 13.
- Chieh-Hsin Lee and F Giuliani, “The Role of Inflammation in Depression and Fatigue.” Front Immunol 10 (2019) 1696-1696.
- Ernst, Mareike, Elmar Brähler, Daniëlle Otten and Antonia M Werner, et al. “Inflammation Predicts New Onset of Depression in Men, but not in Women within a Prospective, Representative Community Cohort.” Sci Rep 11 (2021): 1-12.
- Hayder, Maki, Mazin Jaafar, Thekra A Alkashwan and Ahmed Sudan, et al. “On Admission Levels of High Sensitive C-Reactive Protein as A Biomarker in Acute Myocardial Infarction: A Case-Control Study.”India J Public Health Res Development 10 (2019): 5.
- Qasim Jawad AL-Daami, HSB Ghada H Naji and Hayder AA Makki. “High Sensitivity C-reactive Protein Assessment in Bronchial Asthma: Impact of Exhaled Nitric Oxide and Body Mass Index.” Sys Rev Pharm 11 (2020): 705-711.
- Al-Mumin, Amir, Hayder Abdul-Amir Makki Al-Hindy and Mazin Jaafar Mousa. “Combined Assessments of Multi-panel Biomarkers for Diagnostic Performance in Coronary Artery Disease: Case-Control Analysis.” Sys Rev Pharmacy 11 (2020): 665-671.
- Shaker, Asseel K, Raghdan Al-Saad, Raad Jasim and Hayder Abdul-Amir Makki Al-Hindy. “Biochemical Significance of Cystatin-C and High-Sensitive CRP in Patients with Acute Coronary Syndrome; any Clinical Correlation with Diagnosis and Ejection Fraction.” Sys Rev Pharmacy 11 (2020): 301-308.
- Al-Hindy, Hayder Abdul-Amir Makki, Ali Jihad Hemid Al-Athari and Mazin J Mousa, et al. “The Utility of Serum IL-1 [beta] and CRP Together with Fractional Exhaled Nitric Oxide in the Diagnosis of Asthma in Adults.” Neuro Quantology 19 (2021): 119-124.
- Abdul_Husseein, Hajir Karim, Fouad Sharif Dleikh and Ameera Jasim Al-Aaraji, et al. “Biochemical Causal-Effect of Circulatory Uric Acid, and HSCRP and their Diagnostic Correlation in Admitted Patients with Ischemic Heart Diseases.” J Cardiovascular Dis Res 11(2020): 25-31.
- Raghdan Z, AKS, Dleikh F, Al-Hindy H. “Is There any Association Between Highly Sensitive C-Reactive Protein and Dental-Status in Ischemic Heart Diseases? A Comparative Study.” Biochemical Cellular Arch 20 (2020): 6069-6075.
- Mohammed, Samer Majeed, Aliaa Sameer Hasan, Hayder Abdul Amir Makki Al-Hindy and Mazin J Mousa. “C-Reactive Protein is Associated with the Severity of Periodontal Disease? An Observational Study Among Acute Myocardial Infarction Patients.” Sys Rev Pharmacy 11 (2020): 252-257.
- Danner, Marion, Stanislav V Kasl, Jerome L Abramson and Viola Vaccarino. “Association between Depression and Elevated C-Reactive Protein.” Psychosom Med 65 (2003): 347-356.
- Fond, Guillaume, JA Micoulaud-Franchi, M Faugere and L Boyer, et al. “Abnormal C-reactive Protein Blood Levels as a Specific Biomarker of Major Depression and Non-Remission Under Antidepressants in Schizophrenia.” Prog Neuropsychopharmacol Biol Psychiatry 97 (2020): 109800.
- Maria C Pitharouli, Kylie P Glanville, Jonathan RI Coleman and Matthew Hotopf, et al. “Elevated C-Reactive Protein in Patients With Depression, Independent of Genetic, Health, and Psychosocial Factors: Results From the UK Biobank.” Am Psychiatry 178 (2021): 522-529.
- Ma, Yunsheng, David E Chiriboga, Sherry L Pagoto and Milagros C Rosal, et al. “Association Between Depression and C-reactive Protein.” Cardiol Res Pract 22(2011): 1-9.
- Bordt, Evan A, Caroline J Smith, Tyler G Demarest and Staci D Bilbo, et al. “Mitochondria, Oxytocin, and Vasopressin: Unfolding the Inflammatory Protein Response.” Neurotox Res 36 (2019): 239-256.
- Abdulamir, Haidar A, Omar F Abdul-Rasheed and Emad A Abdulghani. “Low Oxytocin and Melatonin Levels and their Possible Role in the Diagnosis and Prognosis in Iraqi Autistic Children.” Saudi Med J 37 (2016): 29.
- Yasuhiko, Yamamoto and Higashida Haruhiro. “RAGE Regulates Oxytocin Transport into the Brain.” Comm Biol 3 (2020): 1.
- Massey, Suena H, Stephanie A Schuette, Hossein Pournajafi-Nazarloo and Katherine L Wisner, et al. “Interaction of Oxytocin Level and Past Depression May Predict Postpartum Depressive Symptom Severity.” Arch Womens Ment Health 19 (2016): 799-808.
- Sheehan, David V, Yves Lecrubier, K Harnett Sheehan and Patricia Amorim, et al. “The Mini-International Neuropsychiatric Interview (MINI): The Development and Validation of a Structured Diagnostic Psychiatric Interview for DSM-IV and ICD-10.” J Clin Psychiatry 59 (1998): 22-33.
- Kroenke, Kurt, Robert L Spitzer and Janet BW Williams. “The PHQ‐9: Validity of a Brief Depression Severity Measure.” J Gen Intern Med 16 (2001): 606-613.
- NIMH. “Depression Basics”. 5 (2016): 1.
- Osimo, Emanuele Felice, Luke James Baxter, Glyn Lewis and Peter B Jones, et al. “Prevalence of Low-Grade Inflammation in Depression: A Systematic Review and Meta-Analysis of CRP levels.” Psychological Med 49 (2019): 1958-1970.
- Smith, Ronald S. “The Macrophage Theory of Depression.” Med Hypotheses 35 (1991): 298-306.
- Köhler, Cristiano A, Thiago H Freitas, M de Maes and NQ De Andrade, et al. “Peripheral Cytokine and Chemokine Alterations in Depression: A Meta‐Analysis of 82 Studies.” Acta Psychiatr Scand 135 (2017): 373-387.
- Grosse, Laura, Thomas Hoogenboezem, Oliver Ambrée and Silja Bellingrath, et al. “Deficiencies of the T and Natural Killer Cell System in Major Depressive Disorder: T Regulatory Cell Defects are Associated with Inflammatory Monocyte Activation.” Brain 54 (2016): 38-44.
- Fried, Eiko I, S Von Stockert, J MB Haslbeck and F Lamers, et al. “Using Network Analysis to Examine Links between Individual Depressive Symptoms, Inflammatory Markers, and Covariates.” Psychol Med 50 (2020): 2682-2690.
- Beurel, Eléonore, Marisa Toups, and Charles B. Nemeroff. “The Bidirectional Relationship of Depression and Inflammation: Double Trouble.” Neuron 107 (2020): 234-256.
- Horn, Sarah R, Madison M Long, Benjamin W Nelson and Nicholas B Allen, et al. “Replication and Reproducibility Issues in the Relationship between C-Reactive Protein and Depression: A Systematic Review and Focused Meta-Analysis.” Brain Behav Immun 73 (2018): 85-114.
- Haefner, Sibylle, Rebecca T Emeny, Maria Elena Lacruz and Jens Baumert, et al. “Association between Social Isolation and Inflammatory Markers in Depressed and Non-depressed Individuals: Results from the MONICA/KORA Study.” Brain Behav Immun 25 (2011): 1701-1707.
- Nazmi, Aydin, IO Oliveira and Cesar G Victora. “Correlates of C-Reactive Protein Levels in Young Adults: A Population-Based Cohort Study of 3827 Subjects in Brazil.” Braz J Med Biol Res 41 (2008): 357-367.
- Timpson, Nicholas J, Børge G Nordestgaard, Roger M Harbord and Jeppe Zacho, et al. “C-reactive Protein Levels and Body Mass Index: Elucidating Direction of Causation Through Reciprocal Mendelian Randomization.” Int J Obes (Lond) 35 (2011): 300-308.
- Ross, Heather E and Larry J Young. “Oxytocin and the Neural Mechanisms Regulating Social Cognition and Affiliative Behavior.” Front Neuroendocrinol 30 (2009): 534-547.
- Slattery, David A and Inga D Neumann. “Oxytocin and Major Depressive Disorder: Experimental and Clinical Evidence for Links to Aetiology and Possible Treatment.” Pharmaceuticals 3 (2010): 702-724.
- Frasch, A. “Reduction of Plasma Oxytocin Levels in Patients Suffering from Major Depression.” Adv Exp Med Biol 395 (1995): 257-258.
- Miwa, Yusuke, Hidekazu Furuya, Ryo Yanai and Tsuyoshi Kasama, et al. “The Relationship between the Serum Oxytocin Levels, Disease Activity, the ADLs and the QOL in Patients with Rheumatoid Arthritis.” Intern Med (2017): 9191-17.
- Nishi, Daisuke, Kenji Hashimoto, Hiroko Noguchi and Yoshiharu Kim, et al. “Serum Oxytocin, Posttraumatic Coping and C-Reactive Protein in Motor Vehicle Accident Survivors by Gender.” Neuropsychobiology 71 (2015): 196-201.
- Yukselmis, Ozkan. “Serum Oxytocin Levels in Patients with Ankylosing Spondylitis and Non-Radiographic Axial Spondyloarthritis and their Association with Disease Activity.” Aktuelle Rheumatologie (2021): 46 400-405.
- Van Londen, Liesbeth, Jaap G Goekoop, Godfried MJ Van Kempen and Ank C Frankhuijzen-Sierevogel, et al. “Plasma Levels of Arginine Vasopressin Elevated in Patients with Major Depression.” Neuropsychopharmacology 17 (1997): 284-292.
- Cyranowski, Jill M, Tara L Hofkens, Ellen Frank and Howard Seltman, et al. “Evidence of Dysregulated Peripheral Oxytocin Release Among Depressed Women.” Psychosom Med 70 (2008): 967.
- Scantamburlo, Gabrielle, Michel Hansenne, Sonia Fuchs and William Pitchot, et al. “Plasma Oxytocin Levels and Anxiety in Patients with Major Depression.” Psychoneuroendocrinology 32 (2007): 407-410.
- Yuan, Lin, Song Liu, Xuemei Bai and Yan Gao, et al. “Oxytocin Inhibits Lipopolysaccharide-Induced Inflammation in Microglial Cells and Attenuates Microglial Activation in Lipopolysaccharide-Treated Mice.” J Neuroinflammation 13 (2016): 1-17.
- Tang, Yan, Yao Shi, Yifei Gao and Xiaomeng Xu, et al. “Oxytocin System Alleviates Intestinal Inflammation by Regulating Macrophages Polarization in Experimental Colitis.” Clin Sci 133 (2019): 1977-1992.
Citation: Joudi, Mitra, Ali Reza Pezhman, Payam Khalafi and Seyyed Hamzeh Seddiq. “Psychological Responses of Quarantine Due to COVID-19 Pandemic in Normal and Autistic Students : A Narrative Study.” Clin Schizophr Relat Psychoses Clin Schizophr Relat Psychoses, Volume 15: S9, 2021 15S(2021). Doi: 10.3371/CSRP.JMAP.010622.
Copyright: © 2022 Joudi M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.