Research Article - Clinical Schizophrenia & Related Psychoses ( 2024) Volume 18, Issue 1
Influence of Sociodemographic, Economical and Employment-Related Factors on Sick Leave Due to Mental Illness: A Retrospective Study in an Industrialized Region in Southern Europe
Fernando Fuertes Guiro1,2*, Carmen Marqués Gaspar2, Ajda Amet2 and Luis Fernández Bengoa32Department of Sick Leave Management, EGARSAT, Mutual Society for Work Accidents and Work-Related Illnesses, Barcelona, Spain
3EAP Canet de Mar, Metropolian Nord Area Barcelona, Catalan Institute of Health, Barcelona, Spain
Fernando Fuertes Guiro, Department of Medicine, International University of Catalonia, Barcelona, Spain, Email: ffuertes@uic.es
Received: 08-Apr-2024, Manuscript No. CSRP-24-131749; Editor assigned: 11-Apr-2024, Pre QC No. CSRP-24-131749 (PQ); Reviewed: 26-Apr-2024, QC No. CSRP-24-131749 (QC); Revised: 03-May-2024, Manuscript No. CSRP-24-131749 (R); Published: 10-May-2024, DOI: 10.3371/CSRP. GFCG.051024
Abstract
Background: This study identifies and analyzes based on a retrospective descriptive study of a labor Mutual insurance Company Society in the field of the industrialized region of southern Europe (Catalonia), those var iables that may influence sick leave due to mental illness.
Methodology: All workers who were on sick leave during the period 2009-2019 due to mental illness were included in the study. Relationships between social/ employment-related and economical and demographic factors were analyzed using multivariate logistic regression and the multipl e linear regression models.
Results: The period studied included 34,764 workers. Anxious-depressive disorders account for 83.3% of the diagnosed mental disorders. The age cohorts between 30 and 50 years represent 60% of the affected workers. Highest income and high population density regions are the most affected. The levels of mental illness are higher in spring and summer. The years of the economic crisis reduced the amount of sick leave due to mental illness. Professions related to manufacturing industry, automobile mechanics companies, the hospitality industry, teaching and healthcare and social service companies was more heavily affected.
Conclusions: Population density and GDP per capita, the age cohort, the season of the year, the type of payment, the type of contract, and the worker’s business and profession can predict the appearance of sick leave due to mental illness. MICshould plan interventions to minimize these factors and avoid the socioeconomic consequences.
Keywords
Sick leave • Mental illness • Predictors • Prevention
Abbrevations
MIC: Mutual Insurance Companies; SL: Sick Leave; HR: Hazard Ratio; ICD 9: International Classification of Diseases 9; NCBA: National Code of Business Activities; NOC: National Occupation Code
Introduction
Temporary disability is a situation in the working life of workers which is very difficult to evaluate, with a high incidence and repercussions on a country’s social, economic, political and business environment.
Mental illnesses are considered one of the causes of long-lasting and recurrent sick leave, and permanent disability in its various forms [1-3]. These data are a reflection of the pandemic nature of these illnesses in the contemporary world: Anxiety disorders, dissociative and somatoform disorders, and depressive disorders are the second ranked cause of sick leave due to common illnesses in Spain and the third ranked in Europe [4,5]. According to various studies, their prevalence is calculated at between 15 and 25% of causes of primary healthcare appointments, where sick leave certificates are issued [6].
The economic implications of sick leave due to mental illness is the second highest cost to the public purse [7]. In addition, once the patients return to work, their new situation affects their performance. Meanwhile, some companies cannot accept these workers until their treatment has finished and there are no indications that their situation will have a negative impact on their working environment (e.g. commercial airlines, companies undertaking hazardous work).
Psychosocial risk factors for the development of mental illness have been extensively studied in the scientific literature [8-13]. In specific terms, area of activity and occupation, age, differences between countries and socioeconomic status have been associated with the impact on the incidence of mental illness. However, the search for and the relationship between variables that influence sick leave in terms of mental illness is limited, with little evidence reported.
A systematic review from 2011 identifies the following more or less consistent risk factors o predictors for sick leave due to mental illness: Age, history of previous sick leave, negative recovery expectation, socioeconomic status, unemployment, and quality and continuity of occupational care [14]. Other studies have associated sick leave due to mental illness to other factors: Level of education, gender, poor employment conditions, sociodemographic factors-living alone, residing outside big cities, the employer’s economic activity and type of social security contributions and type of contract [15-20]. Meanwhile, some socioeconomic outcomes have been addressed in the literature, which has highlighted the influence of inequalities and economic differences among workers on SL due to mental illness [21-23]. This scientific evidence often covers mental illnesses as a whole more than each specific mental pathology, although illnesses related to affective symptoms known as common mental disorders (anxiety and depression), and alcohol abuse and dependence have been the most widely studied [24].
Mutual Insurance Companies (MIC) working with the National Institute for Social Security (NISS) are non-profit institutions overseen by the Spanish Ministry of Employment and Social Security. Sick leave situations are managed by the NISS, normally working with the network of mutual insurance healthcare providers for occupational accidents and illnesses. These MIC provide occupational healthcare, and are also responsible for the ongoing medical follow-up of patients on sick leave not related to an occupational accident or disease, in order to prevent absence from work due to unnecessary or prolonged illness.
Even taking into account the high incidence and prevalence of mental illness and its impact on temporary disability in employment as well as the progress made in its prediction, more studies to identify new predictors are still needed (and also those related to different regions in the world), and to reinforce the scientific evidence from those already identified. Workers with these pathologies (some more than others) are known to have a higher risk of absenteeism and of poorer performance at work after returning. This study is presented with this in mind.
Based on retrospective information of 34,764 patients with sick leave due to mental disorders according to IDC9 obtained over a period of 10 years from a database of a mutual insurance NISS healthcare provider in an industrialized region in Southern Europe (Catalonia), this study sought to identify and evaluate variables that may influence sick leave due to mental illness based on the following objectives.
Identification, selection and processing of three groups of variables: sociodemographic (gender, age, age cohort, GDP per inhabitant and population density); employment-related (month of start of SL, month of return to work, year of SL, cause of return to work, duration of SL) and economic (type of payment, type of social security contribution, activity of the company and occupation of the worker).
Descriptive study of the variables selected for each mental pathology for each IDC9 group in the insured employed population selected for the period analyzed.
Evaluation of the influence of each variable on the prediction of absenteeism from work for each group of mental disorder in the working population studied.
Materials and Methods
Selection of the study population
This study was carried out at the Mutua Egarsat, a mutual insurance company working with the Spanish National Social Security Institute. In 2018, Egarsat had 35,034 member companies to cover occupational injuries and illnesses, and 23,910 companies for non-work-related injuries or illnesses. In total, the mutual insurance company covers 291,10 3 workers.
All the diagnoses of patients included in the computerized records of the mutual insurance company Egarsat who were on sick leave due to mental illness between January 2009 and June 2019 were included in the study, based on the diagnoses coded according to ICD-9. It is estimated that the sample size will enable detection of differences with a probability greater than 90% with a bilateral significance of 5% (HR 1.21).
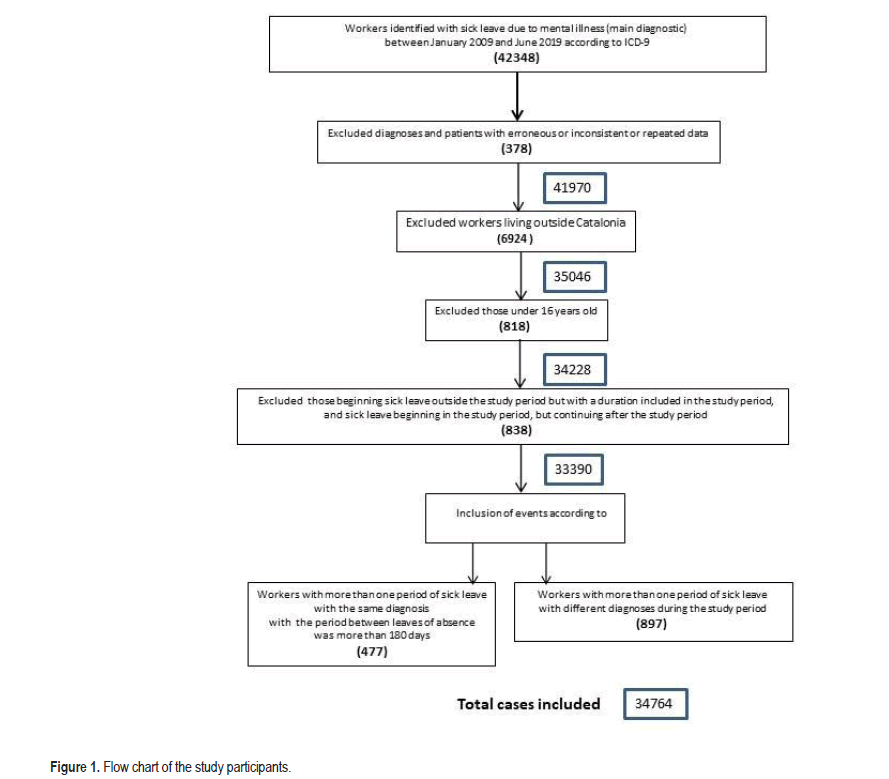
The following were excluded from the study: a) diagnoses and patients with erroneous or inconsistent or repeated data, b) workers living outside Catalonia, c) those under 16 years old, d) those beginning sick leave outside the study period but with a duration included in the study period, e) Sick leave beginning in the study period, but continuing after the study period. Only the events that started and ended in the study period were therefore included in the study. Other selection criteria were: a) workers with more than one period of sick leave with the same diagnosis during the study period were considered as new events if the period between leaves of absence was more than 180 days; otherwise, a single period of sick leave was considered, and b) workers with more than one period of sick leave with different diagnoses during the study period were considered as different events, regardless of the time elapsed between episodes or illnesses), c) Selection of the main diagnoses in each illness.
Ethical-legal considerations
As this is a retrospective descriptive study of computerized patient data, it was not necessary to obtain informed consent from the workers who are the subject of this study. All the data obtained was treated with the confidentiality stipulated in the current legislation. All procedures designed and used in this study comply with the ethical standards of Spanish and International organizations and committees and with the 1975 Declaration of Helsinki and its 2008 revision.
Data collection
All the diagnoses of mental illness according to International Statistical Classification of Diseases and Related Health Problems (ICD 9, Spanish) were obtained from the general Egarsat database. Once obtained, they were adapted to the working population and the number of records for each pathology to be studied by ICD 9, providing the diagnostic groups: Schizophrenic disorders (diagnostic group, 295); Episodic mood disorders (296); Delusional disorders and other nonorganic psychoses (diagnostic groups 297 and 298); Anxiety, dissociative and somatoform disorders (diagnostic group 300); Personality disorders and disturbance of conduct not elsewhere classified (diagnostic groups 301 and 312); Alcohol dependence síndrome (diagnostic group 303); Drug dependence and nondependent abuse of drugs (diagnostic groups 304 and 305); Special symptoms or syndromes not elsewhere classified and physiological malfunction arising from mental factors (diagnostic goups 306 and 307); Acute reaction to stress (diagnostic group 308); Depressive disorder not elsewhere classified (diagnostic group 311).
The independent variables of mental events or illnesses (dependent variables) considered in this study were classified into 3 groups as follows:
Sociodemographic independent variables
• Population and region: The workers were grouped by Catalan region according to GDP per inhabitant and population density, based on the municipality where their declared domicile was located in the Catalan territorial organization of 2015 (containing 42 regions).
• Age: The worker's exact age when the period of sick leave began.
• Age cohort: In order to carry out the statistical study with more approximate demographic data, six cohorts were designed for this study: ≤ 20 years, 20-29 years, 30-39 years, 40-49 years, 50-59 years, ≥ 60 years.
• Gender: Dichotomous variable-male/female.
Employment-related independent variables
• Month of start of sick leave: Numbered from 1 to 12.
• Month of return to work: Numbered from 1 to 12.
• Year of the beginning of sick leave.
• Duration of the sick leave, in days.
• Cause of return to work after sick leave: Healing, Death, Medical inspection, Improvement that allows work, Administrative.
Economic predictive variables
Type of payment during the sick leave period. There are three possible situations: 1. Delegated payment (the company pays the worker the financial benefits during the sick leave period); 2. Direct payment (the mutual insurance company pays the worker, in cases of self-employed workers or those are ineligible for the delegated payment from the beginning of the sick leave period); 3. Loss or termination of the delegated payment, while the worker is still on leave from work, leading to direct payment (the mutual insurance company is responsible for the financial benefit).
• Type of contrac: General system, self-employed and others..
• Profession of the worker, as defined by the National Occupation Code (NOC, 1994) [24]. These were classified into 10 groups.
• Company’s business activity, according to the classification of the National Code of Business Activities (NCBA, 2009) [25]. These were classified in 21 groups.
Statistical analysis
Descriptive statistics will be obtained for each of the selected variables.
The categorical variables (dichotomous and ordinal) are expressed as numbers with corresponding percentages. The continuous variables are expressed as means with standard deviations, or in the case of nonparametric data, as medians with Interquartile Ranges (IQR). Continuous numeric variables will be transformed into categorical ordinals where possible.
Multivariate logistic regression will be used to estimate the effect of each predictor variable on each mental pathology group when the response variable is categorical (adjusted Odds Ratios (ORs) and their 95% confidence intervals will be reported), and the multiple linear regression model will be used for the continuous variable numerical respon se.
The following indicators will be used to assess the goodness of fit and predictive power of each regression: The Chi Squared test (Fisher's exact test, if applicable) for categorical data and Coefficient determination R2 for continuous data.
A p ≤ 0.05 will be considered statistically significant. All the statistical analyses will be carried out using the statistical package for social sciences version 23 for Windows (SPSS Inc., Chicago US).
Results
Once the years of study were delimited in the computer system, 42,348 records were obtained, which after filtering with the inclusion and exclusion criteria, were reduced to 34,764 workers, of whom 13,770 (39.6%) were men and 20,994 (60.4%) were women (p<0.05) as shown in Figure 1 .
Descriptive results
The descriptive results of the dependent variable are presented in Tables 1 and 2. Grouped by diagnosis anxiety, dissociative and somatoform disorders account for 76% of the illnesses studied (26,419 cases), episodic mood disorders account for 8.3% and depressive disorders 7.3%.
| Groups of diseases | Events | Days spent on SL | Age when began SL | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N (%) | Mean (SD) | Mean (SD) | |||||||||||
| Schizophrenic disorders | 206 (0.6) | 163.3 (12.5) | 38.9 (8.7) | ||||||||||
| Episodic mood disorders | 2888 (8.3) | 128.1 (9.7) | 44.3 (10.8) | ||||||||||
| Delusional disorders and other nonorganic psychoses | 291 (0.8) | 161.6 (15.5) | 41.6 (10.7) | ||||||||||
| Anxiety, dissociative and somatoform disorders | 26419 (76.0) | 72.4 (10.2) | 40.2 (10.6) | ||||||||||
| Personality disorders and disturbance of conduct not elsewhere classified | 490 (1.4) | 149.3 (14.1) | 41.1 (11.4) | ||||||||||
| Alcohol dependence syndrome | 175 (0.5) | 133.4 (15.9) | 45.0 (9.1) | ||||||||||
| Drug dependence and nondependent abuse of drugs | 297 (0.8) | 167.8 (17.3) | 39.8 (8.7) | ||||||||||
| Special symptoms or syndromes not elsewhere classified and physiological malfunction arising from mental factors | 1039 (3.0) | 35.4 (7.7) | 37.8 (10.6) | ||||||||||
| Acute reaction to stress | 423 (1.2) | 56.99 (7.8) | 41.2 (10.8) | ||||||||||
| Depressive disorder not elsewhere classified | 2536 (7.3) | 150.73 (14.4) | 45.6 (10.5) | ||||||||||
| Age cohort | N (%) | GDP per inhabitant (Thousands Euros) | N (%) | Population density (Hab / Km2) | N (%) | ||||||||
| <20 | 221 (0.6%) | >41 | 7 (0.02%) | <100 | 754 (2.16%) | ||||||||
| 20-30 | 5805 (16.7%) | 35-40 | 7749 (22.3%) | 101-1000 | 7037 (20.24%) | ||||||||
| 30-40 | 11121 (32.0%) | 30-34 | 21398 (61.5%) | > 1000 | 26973 (77.59%) | ||||||||
| 40-50 | 9753 (28.1%) | 25-29 | 2324 (6.7%) | Gender | N (%) | ||||||||
| 50-60 | 6272 (18.0%) | 20-24 | 2775 (7.9%) | Men | 13770 (39.6) | ||||||||
| >60 | 1592 (4.6%) | 15-19 | 513 (1.5%) | Women | 20994 (60.4) | ||||||||
| Month | Month start SL N (%) | Month return to work N (%) | Year start SL | N (%) | Cause return to work | N (%) | |||||||
| January | 2995 (8.6) | 2588 (7.4) | 2009 | 3564 (10.3) | Healing | 69 (0.8) | |||||||
| February | 3144 (9.0) | 2826 (8.1) | 2010 | 2992 (8.6) | Death | 2389 (6.9) | |||||||
| March | 3329 (9.6) | 3257 (9.4) | 2011 | 3003 (8.6) | Medical inspection | 3763 (10.8) | |||||||
| April | 2883 (8.3) | 3073 (8.8) | 2012 | 2504 (7.3) | Improvement that allows work | 22935 (65.9) | |||||||
| May | 3486 (10.0) | 3349 (9.6) | 2013 | 2535 (7.3) | Administrative | 828 (2.4) | |||||||
| June | 3145 (9.0) | 3357 (9.7) | 2014 | 2697 (7.8) | Not documented | 1227 (3.6) | |||||||
| July | 2993 (8.6) | 3398 (9.8) | 2015 | 2902 (8.4) | Recovery professional capacity | 91 (0.3) | |||||||
| August | 1916 (5.5) | 2201 (6.3) | 2016 | 3131 (9.0) | Start home maternity period | 14 (0.0) | |||||||
| September | 3071 (8.8) | 2834 (8.2) | 2017 | 4451 (12.8) | Permanent disability | 3448 (9.0) | |||||||
| October | 3034 (8.7) | 2873 (8.3) | 2018 | 4242 (12.2) | |||||||||
| November | 2833 (8.2) | 2694 (7.8) | 2019 | 2682 (7.7) | |||||||||
| December | 1937 (5.6) | 2314 (6.7) | |||||||||||
Note: SL: Sickness Leave; SD: Standard Deviation.
| Factor | N (%) | |
|---|---|---|
| Type of payment | Delegate payment | 26173 (75.3) |
| Direct payment | 5266 (15.2) | |
| Contract termination during sick leave | 3325 (9.6) | |
| Type of social security contributions | Self employed | 3859 (11.1) |
| General scheme | 30844 (88.7) | |
| Others | 61 (0.2) | |
| NCBA Groups | N (%) | |
| No description | 54 (0.1) | |
| Agriculture. forestry and fishing | 51 (0.1) | |
| Construction of roads and railways | 2239 (6.2) | |
| Domestic workers | 228 (0.6) | |
| Extra-territorial bodies and organisations | 7 (0.0) | |
| Financial leasing | 242 (0.7) | |
| Gambling and betting activities | 743 (2.0) | |
| Legal and accounting activities | 234 (0.6) | |
| Manufacturing | 7492 (20.7) | |
| Mining and quarrying | 6 (0.0) | |
| Other accommodation (host) | 3709 (10.2) | |
| Post-secondary non-tertiary education | 1473 (4.1) | |
| Production of electricity | 6 (0.0) | |
| Public order and safety activities | 1757 (4.8) | |
| Public relations and communication activities | 1429 (3.9) | |
| Renting and leasing of agricultural machinery and | 2241 (6.2) | |
| Repair of communication equipment | 1314 (3.6) | |
| Residential nursing care activities | 3247 (9.0) | |
| Software publishing | 678 (1.9) | |
| Taxi operation | 2101 (5.8) | |
| Waste collection. treatment and disposal activities | 429 (1.2) | |
| Wholesale trade of motor vehicle parts and accessories | 6581 (18.1) | |
| NCO Groups | N (%) | |
| Business management and public administrations | 496 (2.7) | |
| Scientific and intellectual technicians and professionals | 2769 (15.4) | |
| Support technicians and professionals | 6180 (34.3) | |
| Administrative employees | 1938 (10.8) | |
| Restaurant service workers. personnel protection and salesmen of businesses | 2612 (14.5) | |
| Qualified workers of agriculture and fisheries | 216 (1.2) | |
| Artisans and skilled workers in manufacturing. construction and mining industries. except plant and machinery operators | 1808 (10.1) | |
| Plant and machinery operators and assemblers | 1725 (9.6) | |
| Unskilled workers | 254 (1.4) | |
Note: NCBA: National Code of Business Activity, 2009; NCO: National Code of Occupation, 1994.
The age cohorts between 30 and 50 years old account for 60% of the illnesses. The Catalan regions most affected by mental illness were those with highest income levels (GDP of more than € 30,000 per capita) with the 83.84% of the illnesses registered and the regions with a population density greater than 1,000 inhabitants/km2 account for 77.59% of the cases of psychiatric illness observed. The months of the year with the most patients starting sick leave due to mental illness were February, May and June, and the months with the fewest patients starting sick leave were August and December. Meanwhile, March, April, May, June and July were the months with the highest levels of patients returning to work after SL due to mental illness, and August and December with the fewest patients return to work after sick leave.
Among the most common possible reasons for returning to work after mental illness are improvement permitting work (25,938, 74.6%), followed by cure (3,134, 9.0%) and medical inspection (2,389, 6.9%). The distribution of sick leave per year of begining SL was as follows: A progressive decline in the number of sick leave events due to mental illness was observed in the period 2009-2013, while a progressive increase has been verified in the period 2014-2019.
In terms of the type of payment during the period of sick leave, 75.3% of the workers had delegated pay, 15% started and continued their sick leave receiving direct payment, and the remaining 9.6% stopped receiving payment from the company during their sick leave, and then they received direct payment from Mutual health care provider. The employment relationships of patients on sick leave due to mental illness in this study were distributed as follows: 30,847 (88.7%) were employed in the general system, 3,859 (11.1%) were self-employed and 61 (0.2%) had another type of contract.
By NCBA group, the manufacturing industry had more workers on sick leave due to mental illness (7,492, 20.7%), followed by automobile mechanics (6,581, 18.1%), hospitality (3,709, 10.2%), health and social service activities (3,247, 9.0%), and road and rail construction companies (2,239, 6.2%). The business activities with the fewest cases of mental illness were those of electricity production (6,0.01%) and those belonging to offshore organizations (7,0.01%).
By NOC group, support technicians and professionals is the group with the most workers on SL (34.3%), followed by scientific and intellectual technicians and professionals (15.4%) and restaurant service workers, personnel protection and business salesmen (14.5%). In specific terms, the professions related to teaching were the groups that had the highest rates of sick leave due to mental illness in the period observed, with 12.6%, followed by professions related to health, with 7.2% of all professions. Of the total number of records selected by years covered by the study, 17,988 cases of illnesses have NOC codes (51.7% of the total, for the years between 2012 and 2018). The results obtained in the study with this variable are only taken from these data..
By duration in days of sick leave, the mental pathologies with the longest average length of sick leave are drug dependency and nondependent abuse of drugs with 167.8 days, followed by schizophrenic disorders with 163.35 days, and delusional disorders and other nonorganic psychoses with 161.6 days. Mental illnesses with shorter sick leave periods are special symptoms or syndromes not classified elsewhere, and physiological dysfunction due to mental factors with 35.4 days, and anxiety, dissociative and somatoform disorders with 72.4 days on average.
Regarding the age of the worker at the time of starting the SL period, the youngest mean age of the patients was for those with schizophrenic disorders (38.9) and drug dependence/nondependent abuse of drugs (39.8), while for episodic mood disorders and depressive disorder not classified elsewhere, the patients had an older mean age (44.3 and 45.6 years respectively).
Statistical multivariate and linear logistic regression model
Tables 3-5 present the results of the independent variables that were statistically significant in the statistical multivariate and linear logistic regression model.
| Schizophrenic disorders | Episodic mood disor ders | Delusional disorders and other nonorganic psychoses | Anxiety, dissociative and somatofo rm disorders | Personality disorders and disturbance of conduct not elsewhere classified | Alcohol dependence syndrome | Drug dependence and nondepe ndent abuse of drugs | Special symptoms or syndromes not elsewhere classified and physiological malfunction arising from mental factors | Acute reaction to stress | Depressive disorder not elsewhere classified | |
|---|---|---|---|---|---|---|---|---|---|---|
| Population density by Region | OR (CI 95%) p value | OR (CI 95%) p value | OR (CI 95%) p value | OR (CI 95%) p value | OR (CI 95%) p value | OR (CI 95%) p value | OR (CI 95%) p value | OR (CI 95%) p value | OR (CI 95%) p value | OR (CI 95%) p value |
| <100 | 0.56 (0.48-0.67) 0.01 | 2.34 (1.88-2.76) 0.04 | 0.71 (0.46-0.88) 0.04 | |||||||
| 101-1000 | 0.36 (0.29-0.42) 0.00 | 0.21 (0.18-0.25) 0.00 | 1.30 (1.09-1.49) 0.02 | 0.27 (0.23-0.31) 0.01 | ||||||
| >1000 | 1.92 (1.77-2.12) 0.02 | 0.77 (0.69-0.86) 0.01 | 1.89 (1.67-1.98) 0.01 | 0.39 (0.33-0.42) 0.02 | 2.73 (2.49-2.88) 0.00 | 1.45 (1.38-1.54) 0.01 | ||||
| GDP per inhabitant by Region | OR (CI 95%) p value | OR (CI 95%) p value | OR (CI 95%) p value | OR (CI 95%) p value | OR (CI 95%) p value | OR (CI 95%) p value | OR (CI 95%) p value | OR (CI 95%) p value | OR (CI 95%) p value | OR (CI 95%) p value |
| >41 | ||||||||||
| 35-40 | 1.09 (0.96-1.16) 0.01 | 1.96 (1.88-2.07) 0.00 | ||||||||
| 30-34 | 2.73 (2.56-2.89) 0.00 | 0.63 (0.58-0.69) 0.03 | ||||||||
| 25-29 | 0.63 (0.58-0.69) 0.00 | 2.34 (2.21-2.48) 0.03 | ||||||||
| 20-24 | 1.45 (1.33-1.59) 0.00 | |||||||||
| 15-19 | 2.09 (1.89-2.28) 0.02 | |||||||||
| Age cohort | OR (CI 95%) p value | OR (CI 95%) p value | OR (CI 95%) p value | OR (CI 95%) p value | OR (CI 95%) p value | OR (CI 95%) p value | OR (CI 95%) p value | OR (CI 95%) p value | OR (CI 95%) p value | OR (CI 95%) p value |
| <20 | 0.12 (0.09-0.15) 0.03 | 0.11 (0.08-0.14) 0.01 | ||||||||
| 20-29 | 2.11 (1.98-2.23) 0.01 | 0.14 (0.10-0.19) 0.01 | 0.19 (0.15-0.23) 0.01 | 3.94 (3.55-4.23) 0.00 | ||||||
| 30-39 | 0.10 (0.07-0.12) 0.02 | 2.49 (2.33-2.59) 0.00 | 0.41 (0.36-0.45) 0.02 | 0.56 (0.50-0.62) 0.00 | 0.36 (0.31-0.40) 0.02 | 3.46 (3.22-3.54) 0.02 | ||||
| 40-49 | 0.10 (0.08-0.11) 0.01 | 2.05 (1.96-2.12) 0.00 | 0.63 (0.54-0.69) 0.00 | 0.41 (0.35-0.46) 0.03 | 2.29 (2.12-2.38) 0.00 | |||||
| 50-59 | 0.50 (0.43-0.54) 0.05 | 1.51 (1.44-1.61) 0.00 | 0.76 (0.69-0.83) 0.00 | 1.64 (1.54-1.71) 0.00 | ||||||
| Gender | ||||||||||
| Women | 3.45 (3.12-3.77) 0.02 | 1.38 (1.22-1.48) 0.04 | 2.87 (2.77-2.98) 0.02 | |||||||
| Men | 1.78 (1.69-1.90) 0.03 | |||||||||
The goodness of fit was reviewed for the categorical data in each regression, obtaining a non-significant p value which confirmed the goodness of fit of the model. The results were as follows: Psychotic disorders: Chi square 4.34, p 0.34; neurotic disorders (anxiety and dissociative and somatoform disorders): Chi square 1.29, p 0.67; acute reaction to stress: Chi square 2.25, p 0.64; depressive disorders not classified elsewhere: Chi square 2.88, p 0.39, personality disorders and behavior alterations not classified elsewhere: Chi square 2.97, p 0.29; alcohol dependence síndrome: Chi square 1.89, p 0.66; drug dependence and non-dependent drug abuse,: Chi square 3.78, p 0.28; special symptoms or syndromes not classified elsewhere and physiological malfunction arising from mental factors: Chi square 2.03, p 0.48. The results for the continous data are shown in Table 4.
| Schizophrenic disorders | Episodic mood disorders | Delusional disorders and other nonorganic psychoses | Anxiety, dissociative and somatoform disorders | Personality disorders and disturbance of conduct not elsewhere classified | Alcohol dependence syndrome | Drug dependence and nondependent abuse of drugs | Symptoms or syndromes not elsewhere classified and physiological malfunction arising from mental factors | Acute reaction to stress | Depressive disorder not elsewhere classified | ||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Year beginig SL | OR (CI 95%) p value | OR (CI 95%) p value | OR (CI 95%) p value | OR (CI 95%) p value | OR (CI 95%) p value | OR (CI 95%) p value | OR (CI 95%) p value | OR (CI 95%) p value | OR (CI 95%) p value | OR (CI 95%) p value | |
| 2009 | 0.39 (0.32-0.44) 0.01 | 2.47 (2.22-2.57) 0.00 | 0.12 (0.09-0.14) 0.01 | 0.13 (0.010-0.15) 0.00 | |||||||
| 2010 | 2.38 (2.18-2.49) 0.05 | 0.49 (0.40-0.55) 0.00 | 1.55 (1.29-1.67) 0.00 | 0.46 (0.38-0.51) 0.00 | 2.37 (2.17-2.48) 0.00 | 0.68 (0.59-0.74) 0.00 | |||||
| 2011 | 0.47 (0.40-0.54) 0.00 | 0.58 (0.51-0.62) 0.04 | 1.71 (1.66-1.80) 0.00 | 0.32 (0.26-0.39) 0.00 | 2.48 (2.29-2.61) 0.00 | 0.38 (0.32-0.47) 0.04 | |||||
| 2012 | 0.52 (0.44-0.60) 0.00 | 1.65 (1.49-1.71) 0.00 | 0.25 (0.20-0-30) 0.00 | 1.88 (1.69-1.99) 0.00 | 0.25 (0.21-0.29) 0.00 | 1.89 (1.71-1.99) 0.02 | |||||
| 2013 | 0.44 (0.40-0.50) 0.00 | 0.67 (0.62-0.73) 0.03 | 1.61 (1.54-1.67) 0.00 | 0.33 (0.28-0.39) 0.01 | 1.80 (1.72-1.91) 0.00 | 0.50 (0.39-0.58) 0.04 | 1.42 (1.38-1.47) 0.00 | ||||
| 2014 | 0.52 (0.44-0.58) 0.00 | 0.44 (0.39.0-50) 0.04 | 1.37 (1.28-1.50) 0.00 | 0.48 (0.44-0-54) 0.00 | 1.72 (1.63-1.80) 0.00 | 0.38 (0.33-0.41) 0.00 | 2.26 (2.08-2.33) 0.00 | ||||
| 2015 | 0.88 (0.78-0.96) 0.02 | 0.48 (0.41-0.54) 0.01 | 1.22 (1-08-1.32) 0.00 | 0.32 (0.26-0.45) 0.01 | 1.99 (1.82-2.12) 0.00 | 0.30 (0.22-0.39) 0.00 | 1.42 (1.33-1.49) 0.01 | ||||
| 2016 | 2.12 (1.97-2.23) 0.03 | 1.21 (2.12-2.29) 0.01 | 0.19 (0.12-0.23) 0.00 | 1.65 (1.48-1.76) 0.00 | 0.30 (0.22-0.37) 0.00 | 0.70 (0.58-0.81) 0.00 | |||||
| 2017 | 1.32 (1.24-1.39) 0.00 | 0.33 (0.36-0.40) 0.00 | 1.89 (1.76-1.91) 0.00 | 0.44 (0.38-0.51) 0.00 | 0.55 (0.50-0.61) 0.00 | ||||||
| 2018 | 1.52 (1.44-1.60) 0.01 | 1.21 (1.15-1.30) 0.02 | 0.32 (0.24-0.38) 0.03 | 1.42 (1.34-1.48) 0.00 | 0.33 (0.26-0.39) 0.00 | 0.56 (0.47-0.62) 0.00 | |||||
| 2019 | 1.37 (128-1.43) 0.02 | 1.23 (1.17-1.33) 0.01 | 0.41 (0.38-0.50) 0.00 | 1.59 (1.48-1.66) 0.00 | 0.55 (0.48-0.66) 0.00 | 0.57 (0.51-0.66) 0.00 | |||||
| Month of SL Month of RTW | OR (CI 95%) p value | OR (CI 95%) p value | OR (CI 95%) p value | OR (CI 95%) p value | OR (CI 95%) p value | OR (CI 95%) p value | OR (CI 95%) p value | OR (CI 95%) p value | OR (CI 95%) p value | OR (CI 95%) p value | |
| January | SL | 1.67 (1.58-1.75) | |||||||||
| RTW | |||||||||||
| February | SL | 2.66 (2.44-2.71) 0.02 | |||||||||
| RTW | |||||||||||
| March | SL | 2.77 (2.47-2.98) 0.00 | |||||||||
| RTW | |||||||||||
| April | SL | 2.11 (2.02-2.19) 0.01 | |||||||||
| RTW | |||||||||||
| May | SL | 1.76 (1.47-1.77) 0.00 | 0.76 (0.58-0.88) 0.02 | ||||||||
| RTW | 1.27 (1.13-1.39) 0.03 | 0.75 (0.66-0.81) 0.03 | 2.77 (2.58-2.81) 0.05 | 1.49 (1.33-1.54) 0.00 | |||||||
| June | SL | 3.58 (3.23-3.65) 0.00 | 0.81(0.69-0.92) 0.00 | ||||||||
| RTW | |||||||||||
| July | SL | 2.42 (2-29-2.54) 0.00 | 080 (0.77-0.91) 0.00 | 1.61 (1.47-1.86) 0.02 | |||||||
| RTW | |||||||||||
| August | SL | 0.81 (0.70-0.92) 0.00 | 2.32 (2.19-2.42) 0.02 | 0.34 (0.27-0.47) 0.00 | 1.44 (1.33-1.52) 0.04 | ||||||
| RTW | 0.43 (0.33-0.54) 0.00 | ||||||||||
| September | SL | 2.28 (2.12-2.39) 0.02 | 085 (0.69-0.93) 0.02 | 2.52 (2.33-2.64) 0.00 | |||||||
| RTW | |||||||||||
| October | SL | 3.16 (3.02-3.44) 0.00 | |||||||||
| RTW | 0.36 (0.22-0.47) 0.02 | 1.19 (1.08-1.28) 0.03 | 0.33 (0.26-0.44) 0.01 | ||||||||
| November | SL | 2.18 (1.97-2.32) 0.04 | |||||||||
| RTW | 065 (0.55-0.78) 0.04 | ||||||||||
| December | SL | ||||||||||
| RTW | 0.40 (0.29-0.58) 0.03 | ||||||||||
| Duratio n of SL | Model: F(6,271)=2,154, p<0,005, R2=0,729 | ||||||||||
| B (DE) | -0.05 | 0.08 | 0.02 | 0.33 | -0.08 | -0.02 | 0.04 | 0.4 | 0.1 | 0.12 | |
| t | -11.6 | 4.4 | 2.3 | 11.7 | -0.2 | -3 | 2.12 | 11.6 | 11.2 | 3.5 | |
| P value | 0 | 0 | 0 | 0 | 0.59 | 0 | 0.02 | 0.02 | 0 | 0.02 | |
Note: SL: Sickness leave; RTW: Return to work.
Sociodemographic variables: Table 3 presents the results of the multiple logistic regression statistics for the sociodemographic predictors. The model indicates that various socio-demographic characteristics are associated with several groups of mental diseases. Affective disorders due to anxiety and depression and episodic mood disorders are the groups of mental pathologies with the most sociodemographic variables significantly associated with SL, while delusional and personality disorders and alcohol and drug dependence have practically no sociodemographic factors associated with SL. High population density is positively associated with SL due to affective disorders (anxiety and depression) respect regions with low density population and the wealth of the region is significantly associated with SL in some of the mental pathologies analyzed: The richest regions (GDP per inhabitant 40-30) are a risk factor for work absenteeism by workers due to anxiety and acute reaction to stress, while the poorest regions (GDP per inhabitant [15-25]) are risk factors for SL for depressive disorders. As for gender, significantly positive associations have been found in women regarding anxiety disorders, personality disorders and depression disorders and in men for drug dependence and nondependent abuse of drugs.
Employment-related variables: Among the employment related predictors as shown in Table 4, the month of the start of the sick leave period presents the following results: Starting sick leave due to schizophrenic disorders is significantly associated with March, June, July, September, October and November. On the other hand, workers with anxiety disorders significantly do not start their SL period in the summer months (June, July, August and September), while workers with depressive disorders are positively associated with starting their SL period in that season (July and August). The beginning of periods of sick leave due to personality disorders and disturbance of conduct not classified elsewhere is significantly associated with the months of April, May, August and September. The onset of sick leave due to alcohol dependence syndrome is significantly associated with January and February, while workers diagnosed with drug dependence and nondependent abuse of drugs significantly avoid beginning their SL period in August. Schizophrenic disorders, personality disorders, and anxiety states are the pathologies most significantly influenced by the month of onset or end of SL.
The year when the sick leave started has the greatest effect on the association of sick leave due to mental illness. As a result, the likelihood of SL increases significantly in workers with anxiety throughout the period studied. Depression is another pathology with a strong association with a likelihood of SL according to the start year: It increased significantly in 2012-2015, while it declined significantly in 2010 and 2016-2019 .
For the duration of sick leave, Table 4 indicates that workers diagnosed with schizophrenic disorders, alcohol dependence syndrome and personality disorders/disturbance of conduct not classified elsewhere are associated with significantly reducing the duration of sick leave, while the other diagnostic groups are associated with significantly increasing the duration of sick leave.
Economic variables: For economic variables as shown in Table 5, according to the type of payment, psychotic disorders, drug dependence and nondependent abuse of drug and depressive disorders are positively associated with direct payment while the worker is on sick leave and in 4 other diagnostic groups, all of which are neurotic pathologies the association significantly declines in workers receiving direct payment. This group contains self-employed workers and workers whose company has terminated their employment contract (they are unemployed) since the start of the SL. In addition, there no association with the worker’s type of payment changing during the sick leave period (from delegated to direct, i.e. they are longer paid by the company during the sick leave period) in two diagnostic groups: Personality disorders and disturbance of conduct not classified elsewhere and depressive disorders.
| Schizophrenic disorders | Episodic mood disorders | Delusional disorders and other nonorganic psychoses | Anxiety, dissociative and somatoform disorders | Personality disorders and disturbance of conduct not elsewhere classified | Alcohol dependence syndrome | Drug dependence and nondependent abuse of drugs | Special symptoms or syndromes not elsewhere classified and physiological malfunction arising from mental factors | Acute reaction to stress | Depressive disorder not elsewhere classified | |
|---|---|---|---|---|---|---|---|---|---|---|
| Type of contract | OR (CI 95%) p value | OR (CI 95%) p value | OR (CI 95%) p value | OR (CI 95%) p value | OR (CI 95%) p value | OR (CI 95%) p value | OR (CI 95%) p value | OR (CI 95%) p value | OR (CI 95%) p value | OR (CI 95%) p value |
| Delega te payment | ||||||||||
| Direct payment | 1.21 (1.13-1.28) 0.00) | 1.44 (1.39-1.52) 0.02 | 0.89 (0.72-0.97) 0.01 | 2.11 (1.98-2.28) 0.02 | 2.33 (2.22-2.39) 0.01 | 0.29 (0.20-0.37) 0.02 | 0.53 (0.47-0.59) 0.01 | 2.54 (2.46-2.61) 0.02 | ||
| Contract termination during sick leave | 0.58 (0.50-0.62) 0.01 | 0.80 (0.72-0.88) 0.04 | ||||||||
| Type of social security contributions | OR (CI 95%) p value | OR (CI 95%) p value | OR (CI 95%) p value | OR (CI 95%) p value | OR (CI 95%) p value | OR (CI 95%) p value | OR (CI 95%) p value | OR (CI 95%) p value | OR (CI 95%) p value | OR (CI 95%) p value |
| Self employed | 9.79 (7.78-10.38) 0.02 | 31.63 (25.96-37.80) 0.01 | 42.03 (35.23-48.23) 0.00 | 12.78 (10.56-13.96) 0.01 | ||||||
| General scheme | 61.40 (52.34-68.99) 0.00 | 37.23 (31.23-42.34) 0.00 | ||||||||
| NCBA | OR (CI 95%) p value | OR (CI 95%) p value | OR (CI 95%) p value | OR (CI 95%) p value | OR (CI 95%) p value | OR (CI 95%) p value | OR (CI 95%) p value | OR (CI 95%) p value | OR (CI 95%) p value | OR (CI 95%) p value |
| Construction of roads and railways | 0.48 (0.38-0.51) 0.00 | 0.28 (0.21-0-34) 0.00 | ||||||||
| Domestic workers | 1.67 (1.50-1.71) 0.02 | |||||||||
| Extra-territorial bodies and organisations | 0.26 (0.19-0.33) 0.01 | 1.49 (1.38-1.60) 0.01 | 0.34 (0.29-0.41) 0.00 | |||||||
| Financial leasing | 0.09 (0.06-0.12) 0.00 | |||||||||
| Gambling and betting activities | 0.24 (0.17-0.31) 0.01 | 0.67 (0.59-0.73) 0.04 | 1.35 (1.28-1.42) 0.04 | |||||||
| Legal and accounting activities | 5.84 (4.79-6.77) 0.01 | 0.69 (0.59-0.78) 0.01 | ||||||||
| Mining and quarrying | 1.58 (1.47-1.69) 0.04 | 1.84 (1.77-1.91) 0.00 | ||||||||
| Post-secondary non- tertiary education | 1.47 (1.38-1.61) 0.00 | |||||||||
| Production of electricity | 0.68 (0.57-0.81) 0.00 | |||||||||
| Public relations and communication activities | 0.70 (0.58-0.81) 0.00 | |||||||||
| Repair of communication equipment | 2.49 (2.37-2.61) 0.00 | |||||||||
| Residential nursing care activities | 2.73 (2.67-2.87) 0.04 | 2.50 (2.42-2.61) 0.02 | ||||||||
| Taxi operation | 0.66 (0.57-0.74) 0.04 | |||||||||
| Waste collection, treatment and disposal activities | 2.73 (2.57-2.91) 0.04 | 1.25 (1.12-1.32) 0.03 | 0.78 (0.66-0.81) 0.00 | 3.39 (3.12-3.44) 0.02 | ||||||
| Wholesale trade of motor vehicle parts and accessories | 0.25 (0.21-0.32) 0.02 | 0.79 (0.72-0.87) 0.00 | ||||||||
| NCO | OR (CI 95%) p value | OR (CI 95%) p value | OR (CI 95%)p value | OR (CI 95%) p value | OR (CI 95%) p value | OR (CI 95%) p value | OR (CI 95%) p value | OR (CI 95%) p value | OR (CI 95%) p value | OR (CI 95%) p value |
| Administrative and commercial department managers | 4.17 (3.88-4.28) 0.01 | |||||||||
| Electrical Engineers | 0.87 (0.77-0.97) 0.02 | |||||||||
| Business management and public administrations | 4.85 (4.02-5.12) 0.03 | |||||||||
| Manufacturing managers | 0.53 (0.49-0.60) 0.02 | |||||||||
| Accommodation managers | 6.72 (5.78-7.12) 0.04 | |||||||||
Note: NOC: National Code of Occupation, 1994; NCBA: National Code of Business Activity, 2009.
As for the type of contract of workers on SL due to mental illness, if the worker is self-employed there is a significantly positive association with anxiety and depressive disorders and two other diagnostic groups (with similar results for workers employed in the general system): Drug dependence and nondependent abuse of drugs and special symptoms or syndromes not classified elsewhere/physiological malfunction arising from mental factors as shown in Table 5.
The business activity of the companies where the patients on sick leave due to mental illness work also has significant results. The probability of SL due to anxiety disorders increase significantly in extra-territorial bodies and organisations and gambling and betting activities. Legal and accounting activities are associated with high risk of SL due to personality disorders. The probability of SL due to acute reaction to stress increase in workers of repair of communication activities. SL in schizophrenic disorders and alcohol dependence síndrome are positively associated with waste collection, treatment and disposal activities. Finally, the probability of episodic mood disorders increases significantly among administrative and commercial department managers as shown in Table 5.
Discussion
The most common causes of SL due to common illness in Spain are psychiatric pathologies, osteo-muscular pathologies and oncological pathologies [26,27]. The MIC have been managing SL for common (nonoccupational) illnesses for more than 20 years, and in that time resources have been put in place which rationally monitor the medical justification for these periods of disability.
This descriptive and analytical study has used the database of a regional mutual insurance company over a period long enough to obtain a critical mass of information that provides the most conclusive results possible in the area of predictive factors of SL due to mental illness. Three groups of variables were selected in the methodological design, and some of them were created in order to receive more robust statistica l treatment.
The descriptive results include several important findings. Affective disorders account for more than 75% of all mental disorders, with neurotic disorders (anxiety, depression) being the most common. This diagnostic group is the one which the medical tribunals rule are fit to return to work after a psychiatric examination, which suggests a possible source of rentier absenteeism [28]. The bulk of patients on SL due to mental illness are located in the cohorts aged 30 to 50 years old, which is consistent with the normal distribution of mental illness in the general population, although as will be seen later, no age range determines a greater or lesser probability of suffering from mental illness. Proportional to population density, the most densely inhabited Catalan regions have a higher incidence of SL due to mental illness. The months with the lowest levels of onset of SL cases are during the periods prior to the summer holidays and at the end of the year, and the months with the lowest levels of sick leave due to mental illness are August and December. These data could be attributed to rentier absenteeism during the SL period. On the other hand, the reason for returning to work is mostly (83%) cure or improvement permitting work, compared to 7% of workers who were forced to return to work by the Medical Inspectors. These workers on SL due to non-occupational common illness (2,389) is a part of the rentier group in the mutual insurance company during the period studied. The distribution by year of the sick leave events shows results comparable to a previous study in which during the years of the economic crisis, the number of SL events due to common non-work-related illnesses fell in comparison with the pre and post crisis period [20]. Similar results were found for the other MIC in terms of the proportion of the type of payment during the SL and the type of contract of workers with mental illness: delegated payment predominates over direct payment and workers employed in the general system over self-employed workers. Interestingly, 9.6% of workers had their contract terminated by the company during the period of sick leave (3,325), which is a fairly high proportion, and could be related to the rentier absenteeism that has been mentioned several times in this study [29].
The results according to the activity of the companies have a similar distribution to the official statistics. As a result, the manufacturing industry, the automobile industry, the hospitality industry, and health and social services activities are the groups with the most workers on sic k leave.
The quantitative variables show that psychotic pathologies and alcohol or drug dependence or abuse have a longer duration than neurotic pathologies, and these results are consistent due to the complexity of the evolution of the symptoms and the difficulty involved in stabilization. In neurotic pathologies, and adaptive pathologies in particular, rentier absenteeism is more significant and more patients in this group are referred to the Medical Inspectors to order a return to work, and as such the duration of the SL is also shorter. The average age of patients during sick leave due to mental illness ranges between an average of 30 and 45 years old for each diagnostic group, which is the normal distribution for these diseases during working ages.
After analyzing the results with the statistics proposed, some results obtained in this study of the data from this mutual insurance company (which are relative results, since they only refer to identified illnesses and cannot be extrapolated to the general population) partially corroborate the information available in other studies and statistics [30,31]. In the analysis by region, those with the highest population density are significantly associated with a greater probability of the appearance of more mental illnesses. The probability of appearance of mental illnesses according to age distribution also follows a predefined pattern in the literature, and in general terms and all cohorts except those under 20 years of age have a significant probability of having an affective mental pathology, particularly depression, anxiety and episodic mood disorders [32,33]. Meanwhile, workers aged under 20 years old are unlikely to experience drug abuse without dependency.
The employment related predictors analyzed also present interesting results. The distribution by months indicates that anxiety disorders decline in June, July, August, and September, which are the most common vacation periods, while the probability of SL due to depression increases during the summer months (June, July, and August). Together with other risk factors, this seasonal distribution of neurotic disorders is considered a determinant in the prevalence of these pathologies [34,35]. As regards the month of return to work, the results provide a distribution that is in some cases relevant and well-known [36,37]: The number of patients on SL due to depression declines significantly in May (which is related to the months with the highest probability of SL); in the spring and summer months, the probability of returning to work declines significantly among patients with psychotic pathologies. Other results for this predictor do not suggest an association with the information provided by the most relevant scientific literature.
Some studies have related the increase in SL due to affective mental illness with periods of economic crisis [20]. The results obtained in this study support this information, especially for anxiety and depression disorders and episodic mood disorders during the 2009-2015 cris is.
The type of payment that the worker receives during the period of SL due to mental illness presents important results. In specific terms, workers with direct payment have a higher probability of sick leave due to psychotic diseases and a lower probability due to neurotic diseases. These results can be explained by the fact that anxiety and depression disorders are less common among this type of workers because they have less psychosocial risk at work [38]. This predictor also indicates that when the worker has been diagnosed with a depressive or personality disorder, the probability that the company will not terminate the contract increases. Among affective disorders, depression is known to be the cause of less rentier absenteeism than anxiety disorders and this could act as a curb on the company dismissing the worker during the period of sick leave [39]. Furthermore, depressive disorder is the diagnosis that is most commonly associated with continuation of the SL period.
There are several possible etiopathogenic mechanisms between suffering from a mental disorder and its relationship with work [40]. Exposure to occupational stress related to the lack of an opportunity to use one's abilities leads to fatigue and various mental disorders, such as adaptive disorders. On the other hand, exposure to psychosocial risks at work may contribute to triggering a mental disorder to which the worker is vulnerable, and the psychosocial risk of work acts as a triggering or aggravating factor. This may explain the significantly increased probability of some mental illnesses in specific business activities found in this study.
This study has found two limitations that may be resolved in future studies. The first is the availability of the insured population of the mutual insurance company by region and year in order to obtain the real proportion in the distribution of sick leave due to mental illness with these predictors [41,42]. Despite this, the results are very approximate to those expected without taking into account the insured base population. The second is that the study could be completed with more variables that cannot be obtained in the database for this retrospective study, such as the level of education, social class, and established psychiatric risk factors.
Conclusion
• Diagnostic groups related to neurotic disorders are the most common cause of SL due to mental illness, with the most populated and most rich regions of Catalonia most affected. Meanwhile, neurotic disorders have a shorter average SL period than psychotic disorders.
• Seasonality is observed at the beginning and end of sick leave due to mental illness, and the fewest new episodes of sick leave are recorded in the months prior to the normal vacation periods, and August and December have the fewest cases of returning to work after mental illness. In specific terms, anxiety disorders decline during the summer months, and depression disorders increase in this period, although the number of medical certificates issued for returning to work due to this pathology increases in May. Finally, affective disorders (anxiety, depression and episodic mood) decline during years of economic crisis.
• Self-employed workers are more likely to begin a period of SL due to mental illness than workers employed in the general system.
• Companies with teaching activities at any level, companies in the health and socio-health fields, and manufacturing companies have more workers on SL due to mental illness.
Declaration
Ethics
This article collects data from a database subject to the European Data Protection Law and application for ethics approval was therefore unnecessary.
Acknowledgments
Not applicable
Funding
Not applicable
Consent to participate
Not applicable
Consent to participate
Not applicable
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
FFG: Study conception and design, acquisition of data, analysis and interpretation of data, drafting of manuscript and critical revision of manuscript.
CM: Analysis and interpretation of data and critical revision of manuscript. AA: Analysis and interpretation of data and critical revision of manuscript.
LFB: Study conception and design, acquisition of data, analysis and interpretation of data and drafting of manuscript.
All authors have read and approved the final manuscript.
References
- Delclòs, Jordi, Manel Plana, Silvia García and Dolors Vila, et al. "Duration of Temporary Incapacity for Common Contingency by Diagnostic Groups." Arch Prev Labor Risk 13 (2010):180-187.
- Benavides, Fernando G, Manel Plana, Consol Serra and Ruth Domínguez, et al. "Temporary Incapacity for Common Contingency: Role of Age, Sex, Economic Activity and the Autonomous Community." Span J Public Health 81 (2007): 183-190.
- Roelen, Corne AM, PC Koopmans, R Hoedeman and U Bültmann, et al. "Trends in the Incidence of Sickness Absence due to Common Mental Disorders between 2001 and 2007in The Netherlands." Eur J Public Health 19 (2009): 625-630.
- Romera, I, V Perez, JM Menchón, and H Delgado-Cohen, et al. "Social and Occupational Functioning Impairment in Patients in Partial Versus Complete Remission of a Major Depressive Disorder Episode. A Six-Month Prospective Epidemiological Study." Eur Psychiatry 25 (2010): 58-65.
- Vaez, Marjan, Gunnar Rylander, Åke Nygrenand Marie Åsberg, et al. "Sickness Absence and Disability Pension in a Cohort of Employees Initially on Long-Term Sick Leave due to Psychiatric Disorders in Sweden." Soc Psychiatry Psychiatr Epidemiol 42 (2007): 381-388.
- Ansseau, Marc, Michel Dierick, F Buntinkxand Paul Cnockaert, et al. "High Prevalence of Mental Disorders in Primary Care." J Affect Dis 78 (2004): 49-55.
- Ballesteros Polo, Mónica, Consol Serra Pujadas, José Miguel Martínez and Manel Plana Almuni, et al. "Comparison of the Cost of Temporary Disability due to a Common Contingency in 2006 between the Provinces of Barcelona and Madrid." Span J Public Health 83 (2009): 453-461.
- Duration of Temporary Incapacity for Common Contingency by Diagnostic Groups
- Plaisier, Inger, Aartjan TF Beekman, Ron de Graaf and Johannes H Smit, et al. "Work Functioning in Persons with Depressive and Anxiety Disorders: The Role of Specific Psychopathological Characteristics." J Affect Dis 125 (2010): 198-206.
- Stein, Dan J, Peter Szatmari, Wolfgang Gaebel and Michael Berk, et al. "Mental, Behavioral and Neurodevelopmental Disorders in the ICD-11: An International Perspective on Key Changes and Controversies." BMC Med 18 (2020): 1-24.
- Palmer, Victoria J, Patty Chondros, Donella Piper and Rosemary Callander, et al. "The CORE Study Protocol: A Stepped Wedge Cluster Randomised Controlled Trial to Test a Co-Design Technique to Optimise Psychosocial Recovery Outcomes for People Affected by Mental Illness in the Community Mental Health Setting." BMJ Open 5 (2015): e006688.
- Scott, Kate M, Ali Obaid Al-Hamzawi, Laura H Andrade and Guilherme Borges, et al. "Associations Between Subjective Social Status and DSM-IV Mental Disorders: Results from the World Mental Health Surveys." JAMA Psychiatry 71 (2014): 1400-1408.
- Furber, Gareth, Leonie Segal, Matthew Leach and Catherine Turnbull, et al. "Preventing Mental Illness: Closing the Evidence-Practice Gap Through Workforce and Services Planning." BMC Health Services Res 15 (2015): 1-14.
- Hensing, Gunnel and Rolf Wahlström. "Chapter 7. Sickness Absence and Psychiatric Disorders." Scand J Public Health Suppl 32 (2004): 152-180.
- Cornelius, L R, J J L van der Klink, JW Groothoff and S Brouwer. "Prognostic Factors of Long Term Disability due to Mental Disorders: A Systematic Review." J Occup Rehabil 21 (2011): 259-274.
- Catalina-Romero, Carlos, Paloma Martinez-Munoz, Luis Quevedo-Aguado andMontserrat Ruiz-Moraga, et al. "Predictors of the Duration of Non-Work-Related Sick Leave due to Anxiety Disorders." Gac Sanit 27 (2012): 40-46.
- Sandanger, Inger, Jan F Nygard, Sören Brage and Gunnar Tellnes. "Relation between Health Problems And Sickness Absence: Gender and Age Differences: A Comparison of Low-Back Pain, Psychiatric Disorders, and Injuries." Scand J Public Health 28 (2000): 244-252.
- Royo-Bordonada, Miguel Angel. "The Duration of Work Incapacity and its Associated Factors." Health Gaze 13 (1999): 177-184.
- Mittendorfer-Rutz, Ellenor, Tommi Härkänen, Jari Tiihonen and Jari Haukka. "Association of Socio-Demographic Factors, Sick-Leave and Health Care Patterns with the Risk of Being Granted a Disability Pension among Psychiatric Outpatients with Depression." Plos One 9 (2014): e99869.
- Kokkinen, Lauri, Anne Kouvonen, André Buscariolli and Aki Koskinen, et al. "Human Service Work and Long-Term Sickness Absence due to Mental Disorders: A Prospective Study of Gender-Specific Patterns in 1,466,100 Employees." Ann Epidemiol 31 (2019): 57-61.
- Real, Eva, Lluís Jover, Ricard Verdaguer and Antoni Griera, et al. "Factors Associated with Long-Term Sickness Absence due to Mental Disorders: A Cohort Studyof 7.112 Patients During the Spanish Economic Crisis." Plos One 11 (2016): e0146382.
- Dorner, Thomas E and Ellenor Mittendorfer-Rutz. "Socioeconomic Inequalities in Treatment of Individuals with Common Mental Disorders Regarding Subsequent Development of Mental Illness." Soc Psychiatry Psychiatr Epidemiol 52 (2017): 1015-1022.
- Torvik, Fartein Ask, Eivind Ystrom, Nikolai Czajkowski and Kristian Tambs, et al. "Socioeconomic Status and Sick Leave Granted for Mental and Somatic Disorders: A Prospective Study of Young Adult Twins." BMC Public Health 15 (2015): 1-9.
- Roelen, C A M, W van Rhenen, P C Koopmans and U Bültmann, et al. "Sickness Absence due to Mental Health Disorders-A Societal Perspective." Occupation Med 62 (2012): 379-381.
- Dewa, Carolyn S, Desmond Loong, Sarah Bonato and Hiske Hees. "Incidence Rates of Sickness Absence Related to Mental Disorders: A Systematic Literature Review." BMC Public Health 14 (2014): 1-14.
- General Disposition: Ministry of Economy and Finance. State Offic Newslett (2010).
- Ministry Economy and Finance. BOE Num (2007).
- Quarterly Report Absenteeism Labor. Randstad Res (2020).
- Temporary Disability Statistics. Nat Inst Statist (2024)
- Grau-Lopez, Lara, Constanza Daigre, Alfred Granell and Laia Grau-López, et al. "Risk Factors for Temporary Work Disability." Actas Esp Psiquiatr 44 (2016): 119-124.
- Eaton, William W, Morton Kramer, James C Anthony and Amy Dryman, et al. "The Incidence of Specific DIS/DSM‐III Mental Disorders: Data from the NIMH Epidemiologic Catchment Area Program." Acta Psychiatr Scand 79 (1989): 163-178.
- Vassos, Evangelos, Esben Agerbo, Ole Mors and Carsten Bøcker Pedersen, et al. "Urban–Rural Differences iin Incidence Rates of Psychiatric Disorders in Denmark." Br J Psychiatry 208 (2016): 435-440.
- Kessler, Ronald C, G Paul Amminger, Sergio Aguilar-Gaxiola and Jordi Alonso, et al. "Age of Onset of Mental Disorders: A Review of Recent Literature." Curr Opin Psychiatry 20 (2007): 359-364.
- Kessler, Ronald C, M Angermeyer, J C Anthony, and R de Graaf, et al. "Lifetime Prevalence and Age-of-Onset Distributions of Mental Disorders in the World Health Organization’s World Mental Health Survey Initiative." World Psychiatry 6 (2007): 168-176.
- Roberts, Tessa, Georgina Miguel Esponda, Dzmitry Krupchanka and Rahul Shidhaye, et al. "Factors Associated with Health Service Utilisation for Common Mental Disorders: A Systematic Review." BMC Psychiatry 18 (2018): 1-19.
- Trang, Phan Minh, Joacim Rocklöv, Kim Bao Giang and Gunnar Kullgren, et al. "Heatwaves and Hospital Admissions for Mental Disorders in Northern Vietnam." Plos One 11 (2016): e0155609.
- Morera, A L, and P Abreu. "Seasonality of Psychopathology and Circannual Melatonin Rhythm." J Pineal Res 41 (2006): 279-283.
- Martín, J San Gil, JL González de Rivera and J González González. "Seasonality and Psychopathology." Psyche: JPsychiatry Med Psychol Psychoso 9 (1988): 11-23.
- Silva, M, D M Resurrección, A Antunes, and D Frasquilho, et al. "Impact of Economic Crises on Mental Health Care: A Systematic Review." Epidemiol Psychiat Sci 29 (2020): e7.
- Mingote Adán, José Carlos, Macarena Gálvez Herrer, Pablo del Pino Cuadrado, and M Gutiérrez García, et al. "The patient who suffers from a depressive disorder at work." Occupation Med Safety 55 (2009): 41-63.
- Oliva-Moreno, Juan, Julio López-Bastida, Angel Luis Montejo-González and Rubén Osuna-Guerrero, et al. "The Socioeconomic Costs of Mental Illness in Spain." Eur J Health Econ 10 (2009): 361-369.
- Mur de Víu, Carlos and Jerónimo Maqueda Blasco. "Occupational Health and Mental Health: State of the Art." Occupation Med Safety 57 (2011): 1-3.
Citation: Guiro, Fernando Fuertes, Carmen Marqués Gaspar, Ajda Amet and Luis Fernández Bengoa. “Influence of Sociodemographic, Economical and Employment-Related Factors on Sick Leave Due to Mental Illness: A Retrospective Study in an Industrialized Region in Southern Europe.” Clin Schizophr Relat Psychoses 18 (2024).
Copyright: © 2024 Guiro FF, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.