Research Article - Clinical Schizophrenia & Related Psychoses ( 2022) Volume 0, Issue 0
Factors Effective in Sleep Disturbance of Depression Associated with Diabetes Mellitus Type 2 and Blood Pressure
Roaa Al-Gburi1, Taha H Alnasrawi2, Abeer Ameen Baqer3, Firas Kanawy Hmod Al-aboudy4, Thulfeqar Ahmed Hamza5, Yasir Salam Kari6*, Holya A Lafta7 and Ghadeer Sabah Bustani82Department of Nursing, University of Warith Al-Anbiyaa, Karbala, Iraq
3Department of Medical Laboratory, Dijlah University, Baghdad, Iraq
4Department of Medicine, Altoosi University, Najaf, Iraq
5Department of Medical Laboratory, Al-Mustaqbal University, Babylon, Iraq
6Department of Medical Sciences, Al-Manara College, Maysan, Iraq
7Department of Medical Sciences, Al-Nisour University, Baghdad, Iraq
8Department of Medical Sciences, The Islamic University, Najaf, Iraq
Yasir Salam Kari, Department of Medical Sciences, Al-Manara College, Maysan, Iraq, Email: yasirsalamkarim@uomanara.edu.iq
Received: 05-May-2022, Manuscript No. CSRP-22-62836; Editor assigned: 08-May-2022, Pre QC No. CSRP-22-62836 (PQ); Reviewed: 20-May-2022, QC No. CSRP-22-62836; Revised: 27-May-2022, Manuscript No. CSRP-22-62836 (R); Published: 06-Jun-2022, DOI: 10.3371/CSRP.ARTA.060622
Abstract
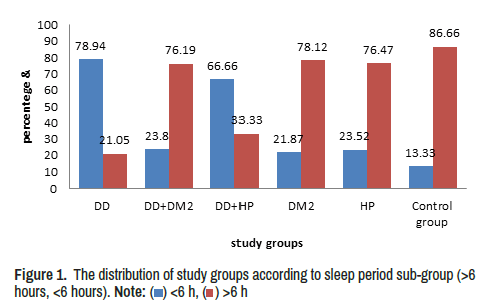
The depression disorder becomes associated with other common diseases that incidence in a high percentage in different populations, the sleep disturbance is found in a high prevalence among individuals. The Current study was suggested to study some factors effecting in the sleep period in depression (DD) associated with diabetes mellitus type 2 (DM2) and blood Pressure (HP). Exercise, diet, family history of disease incidence, Age, duration of disease and BMI which were depended in the current study, the results show there were significant changes in sleep period, Age and BMI among study groups (p=0.000), high percentage of depressed patients and DD+HP (78.95%, 66.66%) respectively have <6 hours of sleeping in significant differences (p=0.000). The other groups have a high percentage of >6 hours of sleeping. The association of sleeping with Exercise, diet, family history shows non-significant impacts except in diet in DD+DM2 that shows significant differences (p= 0.008), the correlation among age, BMI, duration with sleep shows non-significant association, but some correlation changes from positive to inverse relation and vice-versa in comparing with control group as well as age in the DM2, DD+HP and DD+DM2 that have positive correlation with sleep, in duration inverse relation in DD, DD+HP and DM, and in BMI inverse relation in DD, DD+HP and DM2.
Conclusion: These outputs concluded that the different factors' effect may be contributed to sleep disturbance in different diseases in addition to depression disorder infecting patients.
Keywords
Depression • Blood pressure • Hypertension
Introduction
Investigation proved that there was a strong association between sleep disorders and depression and it is considered as important depression symptoms that dependent in diagnoses [1]. Sleep disturbance is a risk of relapse and recurrence when other depression symptoms are ameliorated, it may be led to a few proven risk factors for suicide [2]. The sleep disturbance in depression clinical samples is characterized by difficulty in initiating or maintaining sleep (including early morning waking), this observed in about three quarters of depressed patients [3,4].
The abnormalities of sleep in depression happened by disruption in both homeostatic and circadian drives to sleep, that occurred frequently for a long time to initiate sleep this is observed in other psychiatric conditions, like generalized anxiety disorder [5].
One of the most common comorbidity in diabetes patients is depression [6,7]. The Poor quality of sleep is another common feature of DM2 [8]. Studies were documented that more than half of DM2 suffered from poor sleep quality [9]. The quality of sleeping related to predicting the quality of life in DM2 with controlling for age, duration of disease, type of comorbidities and complications, in addition to insulin use, and depressive symptoms [9,10].
Studies suggested that depression patients have a higher risk for hypertension developing, that lead to predispose to stroke and ischemic heart disease [11,12], also, studies found relation between depression and Masked Hypertension (MHT) and that increases both morning and night- time [13-15]. The present study aims to compare between depression patients, depression with DM2, and depression with HP, DM2, and HP and control group in sleep disorders in some Iraqi cases as a pilot study.
Methodology
The present study enrolled six groups, including depression disorder patients, depression with diabetes mellitus type 2 patients, depressed patients with hypertension, and diabetes mellitus type 2 patients, hypertension patients and healthy individuals male as a control group. All study groups were diagnosed by specialist psychiatry in Al-Sader hospital city, and by glycemic parameters and blood pressure, all data were collected after approval from each contributor. Data included sleep period, age, BMI, exercise activity, diet and family history of disease. Data were represented as mean ± SE, ANOVA one way was used at p<0.05 for significantly detection. Two sub-groups were dependent belong to sleep period in study cases including (>6 hours and <6 hours of sleep) [16].
Results and Discussion
Diabetes mellitus, hypertension and depression become the most common health problems among Iraqi individuals in the last decade [17], thus the current study was suggested to establish the sleep period effective in depression associated with DM2 and hypertension in some Iraqi cases in addition to DM2 and HP groups. Results show that there were significant differences in the sleep period (p=0.000) in depression and depression with HP in comparison with other groups, also significant differences in age (p=0.000) and BMI (p=0.001) (Table 1).
| Groups | AGE | BMI | Duration of disease | Sleep |
|---|---|---|---|---|
| Depression | 35.81 ± 3.11a | 24.8 ± 1.082a | 5.78 ± 1.12 | 4.43 ± 0.70a |
| Depression with DM2 | 48.00 ± 3.10b | 26.72 ± 0.97a | 4.92±1.26 | 7.33 ± 0.42b |
| Depression with hypertension | 50.33 ± 3.179b | 25.66 ± 0.26a | 17.66±1.763 | 4.66 ± 7.88a |
| DM2 | 45.09 ± 2.24b | 30.44 ± 1.22b | 4.28±0.68 | 7.72 ± 0.53b |
| Hypertension | 52.64 ± 2.46c | 29.72 ± 1.10b | 6.56 ± 1.51 | 8.47 ± 0.55b |
| Control group | 33.10 ± 2.07a | 28.06 ± 0.98b | - | 8.10 ± 0.25b |
| Sig | 0.000 | 0.001 | 0.381 | 0.00 |
The associations of depression with other disease have been established by several documents, that clarified the comorbid of diabetes with depression lead to have more diabetes complications and greater dysfunction and worse life quality in compared with patients with normal mood states. Depression with diabetes also represents increased health care costs [18-27].
Two sub-group were depended in a current study according to sleep period (>6 hours and<6 hours), the DD group and DD+HY have higher percentages of (<6 hours) (78.94%, 66.66%) respectively, others groups have high percentages of (>6 hours) in significant differences (X2 26.41, p=0.000) (Figure 1).
The distribution of study groups according to sleep period sub-group (>6 hours, <6 hours) Current study found an association between sleep and depression patients, this result agrees with other studies observed that depression and Sleep disorders are in close relationship, and The epidemiological study clarified that more than 90% of DD will have a sleep disorder, and have difficulties falling asleep, awaken frequently during the night, awaken early, and experience non-refreshing sleep [28,29].
There wasn’t association between DD patients with DM2 and sleep period that didn’t agree with Schipper et al., [30] who conclude that sleep disorders are highly prevalent in DM2 people and negatively affecting health outcomes. Other investigations have shown insomnia to be related DD patients suffered from DM2 (OR 1.31) [31], Same results have been observed in the DM2 and HP groups in the current study, however, in people with DM or HP, the insomnia is associated with an increased mortality rate (OR 7.17) [32].
The factors impact in the sleep period including exercise, diet, and family history of disease were detected, Table 2 clarified that the diet significant effect in the sleep period in DD+DM2 (p=0.008) and control group (p=0.05), while didn't effect on other groups. The exercise non-sig increasing the sleep time in DD+HP, DD, DM2 , groups with family history of disease causing increment in sleep period than groups didn’t have family history.
| Sleep period | DD | DD+DM2 | DD+HP | DM2 | HP | Control | |
|---|---|---|---|---|---|---|---|
| Exercise | |||||||
| No | 4.00 ± 0.63 | 7.23 ± 0.52 | 3.00 ± 1.00 | 7.00 ± 0.87 | 8.44 ± 0.8 | 8.00 ± 0.62 | |
| Yes | 6.25 ± 1.750 | 7.75 ± 0.25 | 8.00 ± 0.009 | 8.45 ± 0.56 | 8.50 ± 0.82 | 8.13 ± 0.28 | |
| sig | 0.152 | 0.648 | 0.212 | 0.177 | 0.962 | 0.821 | |
| Diet | |||||||
| No | 4.50 ± 0.66 | 6.200 ± 0.66 | 5.00 ± 3.00 | 8.14 ± 0.63 | 9.09 ± 0.719 | 7.60 ± 0.43 | |
| Yes | 4.00 ± 0.009 | 8.36 ± 0.33 | 4.00 ± 0.02 | 7.00 ± 0.94 | 7.33 ± 0.714 | 8.60 ± 0.23 | |
| Sig | 0.866 | 0.008* | 0.879 | 0.312 | 0.135 | 0.05* | |
| Family history | |||||||
| No | 4.18 ± 0.70 | 7.92 ± 0.36 | 2.00 ± 0.009 | 8.50 ± 0.70 | 8.25 ± 0.68 | 8.11 ± 0.30 | |
| Yes | 6.00 ± 1.15 | 6.37 ± 0.88 | 6.00 ± 2.00 | 7.28 ± 0.72 | 9.00 ± 1.00 | 8.00 ± 0.09 | |
| Sig | 0.309 | 0.078 | 0.454 | 0.282 | 0.556 | 0.883 | |
Studies clarified that the Exercise has long been associated with better sleep [33]; the available evidence suggests that exercise holds promise as a non-pharmacologic therapy for adults with poor or disordered sleep [34], the Exercise training also lowering in the severity of sleep-disordered breathing, with obstructive sleep apnea the most common type of severity of sleep-disordered examined [35]. A meta-analysis of five studies found that exercise training reduced severity of obstructive sleep apnea by 32% despite a non-significant decrease in BMI.
The diet showed significant effect in the sleep period in current study in the DD+DM2, investigations found the role of Dietary nutrition in sleeping wellness. Several nutritional supplements were used trying to benefit sleep wellness, on the other hand the relationship between sleep and nutritional is complicated, the Nutritional factors diverted with different dietary patterns and depend on the individuals digestive and metabiotic functions. Furthermore, nutrition can effect on the hormones and inflammation status which directly or indirectly contribute to sleep disorder, the carbohydrates, amino acids, lipids and vitamins have effects on sleep in different ways in addition to the health state and chronic disease [36].
The family history of disease in current finding didn't effect in the sleep period, another DM study found there was difficult maintaining or initiating sleep was slightly less than the risk of having a family history of DM [37], the family history of insomnia has a potential role in sleep in different diseases like depression [38], the family history need further examine to prove its relation with different diseases.
The correlation between sleep period and age, BMI and duration of diseases are shown in Table 3.
| Sleep | age | duration | BMI | |
|---|---|---|---|---|
| DD | r | -0.337 | -0.089 | -0.388 |
| p | 0.202 | 0.744 | 0.138 | |
| DD+DM2 | r | 0.420 | 0.013 | 0.266 |
| p | 0.058 | 0.955 | 0.243 | |
| DD+HP | r | 0.693 | -0.759 | -0.702 |
| p | 0.512 | 0.451 | 0.505 | |
| DM2 | r | 0.693 | -0.759 | -0.702 |
| p | 0.512 | 0.451 | 0.505 | |
| HP | r | -0.051 | 0.325 | 0.075 |
| p | 0.845 | 0.203 | 0.774 | |
| Control group | -0.079 | 0 | 0.009 | |
| 0.677 | 0 | 0.961 |
The correlation among age, BMI, duration with sleep shows nonsignificant association, but some correlation changes from positive to inverse relation and vice-versa in comparing with control group as well as age in the DM2, DD+HP and DD+DM2that have positive correlation with sleep, in duration inverse relation in DD, DD+HP and DM, and in BMI inverse relation in DD, DD+HP and DM2.
Li et al. found that the sleep disturbances in older adults are multifactorial, like medical and psychiatric conditions, primary sleep disorders, and changes in environment, social engagement, and lifestyle. Belong to BMI, Grandner et al., referred to the relation between sleep and BMI was a linear, where more sleep is associated with lower BMI, furthermore, Sleep is the most sedentary activity, yet may be the only one that protects from weight gain, in addition to all mention above the duration and complication of diseases have impact in the sleep quality and period [39,40].
Conclusion
Sleep period and quality are an important for life quality, different diseases become common in Iraqi population that have effected in sleep. Depression, diabetes mellitus, hypertension and association among them were enrolled in the current study; the outputs concluded that the impact of different factors may be contributed in sleep disturbance in different disease in addition to associated with depression disorder. But these effects limited by diseases progression, lifestyle and medications which need further investigations.
References
- Jindal, Ripu D and Michael E Thase. “Treatment of Insomnia Associated with Clinical Depression.” Sleep Med Rev 8 (2004): 19-30.
[Cross ref] [Goggle scholar] [Pubmed]
- Agargun, Mehmed Yucel, Hayrettin Kara and Mustafa Solmaz. "Sleep disturbances and suicidal behavior in patients with major depression." J Clin Psychiatry 58 (1997): 249-251.
[Cross ref] [Goggle scholar] [Pubmed]
- Hamilton, Max. “Frequency of Symptoms in Melancholia (Depressive Illness).” Br J Psychiatry 154 (1989): 201-206.
[Cross ref] [Goggle scholar] [Pubmed]
- Yates, William R, Jeff Mitchell, A John Rush and Madhukar Trivedi, et al. “Clinical Features of Depression in Outpatients with and Without Co-occurring General Medical Conditions in STAR* D: Confirmatory Analysis.” Prim Care Companion J Clin Psychiatry 9 (2007): 24284.
[Cross ref] [Goggle scholar] [Pubmed]
- Nutt, David J. “Neurobiological Mechanisms in Generalized Anxiety Disorder.” J Clin Psychiatry 62 (2001): 22-28.
[Goggle scholar] [Pubmed]
- Katon, Wayne, Elizabeth HB Lin and Kurt Kroenke. “The Association of Depression and Anxiety with Medical Symptom Burden in Patients with Chronic Medical Illness.” Gen Hosp Psychiatry 29 (2007): 147-155.
[Cross ref] [Goggle scholar] [Pubmed]
- Alonso-Morán, Edurne, Altynai Satylganova, Juan F Orueta and Roberto Nuño-Solinis. “Prevalence of Depression in Adults with Type 2 Diabetes in the Basque Country: Relationship with Glycaemic Control and Health Care Costs.” BMC Public Health 14 (2014): 1-8.
[Cross ref] [Goggle scholar] [Pubmed]
- Skomro, RP, S Ludwig, E Salamon and MH Kryger. “Sleep Complaints and Restless Legs Syndrome in Adult Type 2 Diabetics.” Sleep Med 2 (2001) 417-422.
[Cross ref] [Goggle scholar] [Pubmed]
- Luyster, Faith S and Jacqueline Dunbar-Jacob. “Sleep Quality and Quality of Life in Adults with Type 2 Diabetes.” Diabetes Educ 37 (2011): 347-355.
[Cross ref] [Goggle scholar] [Pubmed]
- Wändell, Per E and Jonas Tovi. “The Quality of Life of Elderly Diabetic Patients.” J Diabetes Complications 14 (2000): 25-30.
[Cross ref] [Goggle scholar] [Pubmed]
- Meng, Lin, Dongmei Chen, Yang Yang and Yang Zheng, et al. “Depression Increases the Risk of Hypertension Incidence: A Meta-analysis of Prospective Cohort Studies.” J Hypertens 30 (2012): 842-851.
[Cross ref] [Goggle scholar] [Pubmed]
- O’Connor, Christopher M, Paul A Gurbel and Victor L Serebruany. “Depression and Ischemic Heart Disease.” Am Heart J 140 (2000): S63-S69.
[Cross ref] [Goggle scholar] [Pubmed]
- Kayano, Hiroyuki, Shinji Koba, Taiju Matsui and Hiroto Fukuoka, et al. “Impact of Depression on Masked Hypertension and Variability in Home Blood Pressure in Treated Hypertensive Patients.” Hypertension Research 38 (2015): 751-757.
[Crossref] [Google scholar] [Pubmed]
- Davidson, Karina, Bruce S Jonas, Kim E Dixon and Jerome H Markovitz. “Do Depression Symptoms Predict Early Hypertension Incidence in Young Adults in the CARDIA Study?.” Arch Intern Med 160 (2000): 1495-1500.
[Crossref] [Google scholar] [Pubmed]
- Cohen, Hillel W, Shantha Madhavan and Michael H Alderman. “History of Treatment for Depression: Risk Factor for Myocardial Infarction in Hypertensive Patients.” Psychosomatic Med 63 (2001): 203-209.
[Crossref] [Google scholar] [Pubmed]
- Nathaniel F Watson, M Safwan Badr, Gregory Belenky and Donald L Bliwise, et al. “Recommended Amount of Sleep for a Healthy Adult: A Joint Consensus Statement of the American Academy of Sleep Medicine and Sleep Research Society.” Sleep 11 (2015): 591-592.
[Cross ref] [Google scholar] [Pubmed]
- Al-Hamzawi, Ali Obaid, Ronny Bruffaerts and Evelyn J Bromet, et al. “The Epidemiology of Major Depressive Episode in the Iraqi General Population.” PloS one 10 (2015): e0131937.
[Cross ref] [Goggle scholar] [Pubmed]
- Öztürk, Zeynel Abidin, Yusuf Yesil, Mehmet Emin Kuyumcu and Esen Savas, et al. “Association of Depression and Sleep Quality with Complications of Type 2 Diabetes in Geriatric Patients.” Aging clinical and experimental research 27, no. 4 (2015): 533-538.
[Crossref] [Google scholar] [Pubmed]
- Egede, Leonard E. “Diabetes, Major Depression, and Functional Disability among US Adults.” Diabetes Care 27 (2004): 421-428.
[Cross ref] [Google scholar] [Pubmed]
- Kohen, D, AP Burgess, J Catalan and A Lant. “The Role of Anxiety and Depression in Quality of Life and Symptom Reporting in People with Diabetes Mellitus.” Qual Life Res 7 (1998): 197-204.
[Crossref] [Google scholar] [Pubmed]
- Ali, Saima, Margaret Stone, Timothy Chas Skinner and Noelle Robertson, et al. "The Association between Depression and Health‐Related Quality of Life in People with Type 2 Diabetes: A Systematic Literature Review.” Diabetes Metab Res Rev 26 (2010): 75-89.
[Cross ref] [Google scholar] [Pubmed]
- Chyun, Deborah A, Gail D Melkus, Deborah M Katten and Wendie J Price, et al. “The Association of Psychological Factors, Physical Activity, Neuropathy, and Quality of Life in Type 2 Diabetes.” Biol Res Nurs 7 (2006): 279-288.
[Cross ref] [Google scholar] [Pubmed]
- Verma, Swapna K, Nan Luo, Mythily Subramaniam and Chee Fang Sum, et al. “Impact of Depression on Health Related Quality of Life in Patients with Diabetes.” Annals Academy of Medicine Singapore 39 (2010): 913. [Crossref]
[Google scholar] [Pubmed]
- Katon, Wayne, Elizabeth HB Lin and Kurt Kroenke. “The Association of Depression and Anxiety with Medical Symptom Burden in Patients with Chronic Medical Illness.” Gen Hosp Psychiatry 29 (2007): 147-155.
[Cross ref] [Google scholar] [Pubmed]
- Alonso-Morán, Edurne, Altynai Satylganova and Juan F Orueta, et al. “Prevalence of Depression in Adults with Type 2 Diabetes in the Basque Country: Relationship with Glycaemic Control and Health Care Costs.” BMC Public Health 14 (2014): 1-8.
[Crossref] [Google scholar] [Pubmed]
- Manber, Rachel and Andrea S Chambers. “Insomnia and Depression: A Multifaceted Interplay.” Curr Psychiatry Rep 11 (2009): 437-442.
[Crossref][Google scholar] [Pubmed]
- Liao, CZ. Feng, D Zhou and Q Dai, et al. “Dysfunction of Fronto-Limbic Brain Circuitry in Depression.” Neuroscience 201 (2012): 231-23.
[Crossref] [Google scholar] [Pubmed]
- Schipper, Samantha BJ, Maaike M Van Veen, Petra JM Elders and Annemieke van Straten, et al. “Sleep Disorders in People with Type 2 Diabetes and Associated Health Outcomes: A Review of the Literature.” Diabetologia 64 (2021): 2367-2377.
[Crossref] [Google scholar] [Pubmed]
- Nefs, Giesje, Esther Donga, Eus van Someren and Mariska Bot, et al. “Subjective Sleep Impairment in Adults with Type 1 or Type 2 Diabetes: Results from Diabetes MILES—The Netherlands.” Diabetes Res Clin Pract 109 (2015): 466-475.
[Crossref] [Pubmed] [Google scholar]
- Vgontzas, Alexandros N, Duanping Liao, Slobodanka Pejovic and Susan Calhoun, et al. “Insomnia with Short Sleep Duration and Mortality: The Penn State Cohort.” Sleep 33 (2010): 1159-1164.
[Crossref] [Pubmed] [Google scholar]
- Youngstedt, Shawn D and Christopher E. Kline. “Epidemiology of Exercise and Sleep.” Sleep 4 (2006): 215-221.
[Crossref] [Pubmed] [Google scholar]
- Buman, Matthew P and Abby C King. “Exercise as a Treatment to Enhance Sleep.” Am J Med 4 (2010): 500-514.
[Crossref] [Pubmed] [Google scholar]
- Iftikhar, Imran H, Christopher E Kline and Shawn D Youngstedt. “Effects of Exercise Training on Sleep Apnea: A Meta-analysis.” Lung 192 (2014): 175-184.
[Crossref][Pubmed] [Google scholar]
- Zhao, Mingxia, Houzhen Tuo, Shuhui Wang and Lin Zhao. “The Effects of Dietary Nutrition on Sleep and Sleep Disorders.” Mediators Inflamm 2020 (2020) 25.
[Crossref] [Google scholar] [Pubmed]
- Anothaisintawee, Thunyarat, Sirimon Reutrakul, Eve Van Cauter, and Ammarin Thakkinstian. “Sleep Disturbances Compared to Traditional Risk Factors for Diabetes Development: Systematic Review and Meta-Analysis.” Sleep Med Rev 30 (2016): 11-24.
[Crossref] [Pubmed] [Google scholar]
- Beaulieu-Bonneau, Simon, Mélanie LeBlanc, Chantal Mérette and Yves Dauvilliers, et al. “Family History of Insomnia in a Population-Based Sample.” Sleep 30 (2007): 1739-1745.
[Crossref] [Pubmed] [Google scholar]
- Li, Junxin, Michael V Vitiello and Nalaka S. Gooneratne. “Sleep in Normal Aging.” Sleep Med Clin 13 (2018): 1-11.
[Crossref] [Pubmed] [Google scholar]
- Grandner, Michael A, Elizabeth A Schopfer, Megan Sands‐Lincoln and Nicholas Jackson, et al. “Relationship between Sleep Duration and Body Mass Index Depends on Age.” Obesity 23 (2015): 2491-2498.
[Crossref] [Pubmed] [Google scholar]
- Chaput, Jean-Philippe, Lars Klingenberg and Anders Sjödin. "Do all Sedentary Activities Lead to Weight Gain: Sleep Does Not.” Curr Opin Clin Nutr Metab Care 13 (2010): 601-607.
[Crossref] [Google scholar] [Pubmed]
- Stenholm, Sari, Jenny Head, Mika Kivimäki and Linda L Magnusson Hanson, et al. “Sleep Duration and Sleep Disturbances as Predictors of Healthy and Chronic Disease–Free Life Expectancy between Ages 50 and 75: A Pooled Analysis of Three Cohorts.” J Gerontol A Biol Sci Med Sci 74 (2019): 204-210.
[Crossref] [Google scholar] [Pubmed]
Citation: Al-Gburi, Roaa, Taha H Alnasrawi, Abeer Ameen Baqer and Firas Kanawy Hmod Al-aboudy "Factors Effective in Sleep Disturbance of Depression Associated with Diabetes Mellitus Type 2 and Blood Pressure." Clin Schizophr Relat Psychoses 16S (2022) DOI: 10.3371/CSRP.ARTA.060622.
Copyright: © 2022 Al-Gburi R, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.







 ) <6 h, (
) <6 h, (  ) >6 h
) >6 h