Research - Clinical Schizophrenia & Related Psychoses ( 2021) Volume 15, Issue 2
Childhood Trauma and Personal Recovery in Schizophrenia: Mediating Role of Experiential Avoidance and Insecure Attachment
Ricardo M. Hodann-Caudevilla1*, Juan Jesús Muñoz García1* and Francisco Alfonso Burgos Julián22Department of Psychology, King Juan Carlos University, Móstoles, Madrid, Spain
Ricardo M. Hodann-Caudevilla, Department of Psychology, San Juan de Dios Hospital, Ciempozuelos, Madrid, Spain, Email: ricardomiguel.hodann@sjd.es Juan Jesús Muñoz García, Department of Psychology, San Juan de Dios Hospital, Ciempozuelos, Madrid, Spain, Email: ricardomiguel.hodann@sjd.es
Received: 15-Mar-2021 Accepted Date: Mar 29, 2021 ; Published: 05-Apr-2021
Abstract
In recent decade’s interest in the concept of recovery in schizophrenia has grown exponentially. One phenomenon that has been consistently associated with poorer recovery in people with schizophrenia is childhood trauma. The aim of this study is to explore the mechanisms underlying this relationship by analyzing the possible mediating effect of experiential avoidance and insecure attachment.
Method: The sample for this investigation consisted of 109 people with schizophrenia. The assessment employed the following scales: ExpTra- S,AAQ-II, PAM, ISMI and SCIP-S. A Bias-Corrected Bootstrap (BCB) procedure was used in the mediation analysis.
Results: Childhood trauma predicts poorer personal recovery, with experiential avoidance acting as a mediator in this relationship.
Conclusion: People with schizophrenia who have a history of childhood trauma and high levels of experiential avoidance require special clinical attention, with interventions focused on addressing the impact of trauma and on promoting personal recovery.
Keywords
Childhood trauma • Personal recovery • Experiential avoidance • Attachment • Schizophrenia
Introduction
The legacy of the German psychiatrist Emil Kraepelin as a pioneer in the classification of psychiatric disorders and as a promoter of research in the field of schizophrenia is undeniable. However, his view of schizophrenia as a chronic and progressively deteriorating process instilled a therapeutic pessimism that tended to nullify any expectation of recovery [1]. This negative view of the disorder's prognosis continued until the 1980s, when autobiographical accounts began to be published in which affected individuals described how they had managed to cope with the problems associated with schizophrenia, thereby achieving a fulfilling and meaningful life [2]. Thus the concept of recovery emerged in the mental health field.
Recovery in schizophrenia can be analyzed from an objective perspective or from a subjective perspective [1]. Both conceptions share the notion of an improvement within the disorder but differ in a number of key respects. Objective recovery–commonly referred to as clinical recovery implies a reduction in symptoms and an improvement in psychosocial functioning, both of which are assessed by an expert observer. Subjective recovery, or personal recovery, concerns an individual process through which the person learns to manage symptoms and their repercussions in order to build a meaningful and globally satisfying life [3]. Therefore, this view of recovery as a personal subjective process does not allude to a reduction in symptoms and its measurement is based on the assessment of different dimensions related to health and well-being such as hope, relationships, empowerment or quality of life [4]. Two dimensions which are recognized for their involvement in personal recovery are Psychological Quality of Life (Psy-QoL), which refers to the patient's personal judgement of their own well-being [5] and Internalized Stigma (IS), which refers to the patient's perception of themselves as a person with a mental disorder [6].
A phenomenon that has attracted a great deal of interest in the field of clinical psychology in recent decades and that is consistently associated with poorer recovery in people with schizophrenia is childhood trauma. On the one hand, epidemiological studies show a high prevalence of childhood trauma in people with schizophrenia [7]. On the other hand, such type of trauma has been found to be associated with indicators of poorer clinical recovery, like greater severity and persistence of psychotic symptomatology [8]. The available evidence regarding the effects of childhood trauma on dimensions of personal recovery is sparse.
Another factor associated with poorer clinical recovery in schizophrenia is impairments in emotional regulation processes [9]. Several studies have reported that people with psychosis tend to use experiential avoidance-a maladaptive emotional regulation strategy that involves a resistance to tolerate unpleasant experiences and intense efforts to eliminate or reduce internal discomfort [10] – to a greater extent than the non-clinical population [11]. Moreover, its use has been linked to greater positive symptomatology and lower quality of life [12,13]. Experiential avoidance is also frequently observed in survivors of childhood trauma and is associated with elevated levels of psychological distress [14]. However, the possible role of experiential avoidance in the relationship between childhood trauma and recovery from schizophrenia has not been studied to date.
Finally, a high prevalence of insecure attachment has been found in people with schizophrenia compared to people without the disorder (78% and 38%, respectively) [15]. Within the field of psychopathology, insecure attachment has been associated with greater intensity of psychotic symptomatology, poorer social functioning and lower quality of life [15,16]. In the trauma field, a close relationship has been found between childhood trauma and the development of insecure attachment [17]. The fact that poorer recovery in people with schizophrenia is associated with a high prevalence of both childhood trauma and insecure attachment suggests that the three phenomena may be connected, although this possibility has so far not been studied.
Therefore, the aim of this article is to examine whether a history of childhood trauma negatively influences personal recovery in people with schizophrenia spectrum diagnoses and, in addition, to study the possible mediating influence of experiential avoidance and insecure attachment on this relationship. It is hypothesized that, in line with previous research findings, the presence of childhood trauma will predict poorer personal recovery as measured by IS and Psy-QoL (Hypothesis 1). It is also hypothesized that this relationship will be mediated by the level of experiential avoidance (Hypothesis 2) and levels of insecure attachment (Hypothesis 3).
Methodology
Participants
The sample for this study was formed with patients recruited in the Mental Health area of the San Juan de Dios Centre in Ciempozuelos (Madrid). The participants were mostly male (93.6%), with an age range between 22 and 64 years (mean=47.6; SD=9.7), and all of them had been diagnosed with schizophrenia spectrum disorders (paranoid schizophrenia, 68%; residual schizophrenia, 27%; schizoaffective disorder, 10%; delusional disorder, 4%) of at least three years of evolution (Table 1). The mean duration of the disorder was 26.1 years (SD=10.5). Participants, who were in long-term inpatient hospitalization, were recruited by their psychiatrist or clinical psychologist. All were receiving treatment during the study, both pharmacological and psychological. The mean antipsychotic dose that participants were receiving during the study –transformed into haloperidol equivalent doses according to the criteria of Leucht, et al. [18], was 25 mg/ day (SD=15). The research received approval from the Research Ethics Committee (CEIm) of the University Hospital 12 de Octubre (19/117) and all participants gave informed consent. Upon receipt of this approval, data collection began and lasted four and a half months.
Patients were excluded from the study if they had neurological disorders or a moderate, severe or profound intellectual disability. Participants were also excluded from the study if, due to their cognitive status at the time of data collection, they were unable to understand or answer the questions on the questionnaires. The final sample consisted of 109 participants, mostly males (93.6%), with an age ranged from 22 to 64 years (M=47.6; SD=9.7).
Measures
Traumatic experience screening questionnaire for patients with severe mental disorders: (ExpTra-S) [19]. The ExpTra-S is an instrument that allows the assessment of traumatic experiences in childhood in patients with diagnoses of the psychotic spectrum. It consists of two subscales, one for frequency and one for distress, both of which are composed of 18 items. The frequency subscale measures the presence of five types of traumatic experiences in childhood: sexual abuse, physical abuse, emotional abuse, emotional neglect and physical abandonment. The last item on this subscale refers to any type of traumatic event not contained in the previous items. The distress subscale, on the other hand, allows for the assessment of the distress associated with each traumatic experience. Given the objectives of this study, data from the distress subscale were not used. The authors of the questionnaire reported adequate psychometric properties in terms of internal consistency (Cronbach's α=0.96) with all discrimination indices above 0.30.
Acceptance and Action Questionnaire–II (AAQ-II): To measure experiential avoidance, the AAQ-II questionnaire was used in its version adapted to Spanish and validated by Ruiz, et al. [20,21]. It consists of seven items whose content refers to resistance to experiencing unwanted emotions and thoughts, as well as the inability to be in the present moment and perform value-driven actions in the presence of aversive internal events. The version used has a high internal consistency (α between 0.75 and 0.93) and adequate parameters of convergent validity.
Psychosis Attachment Measure (PAM): The PAM is a 16-item questionnaire that allows the assessment in people with psychotic spectrum disorders of two dimensions of adult attachment: Anxiety and avoidance. The version adapted to Spanish and validated by Sheinbaum, et al. [22,23] was used. Unlike most instruments that measure adult attachment, it is applicable to individuals who do not maintain –or who have never had– a romantic relationship at the time of the assessment. Sheinbaum, et al. [23] reported that their version of the scale maintains the factorial structure of the original one and presents high reliability (α=0.81 for the anxiety subscale and α=0.78 for the avoidance subscale), as well as good convergent validity.
Short form health survey: The SF-36 questionnaire provides a measure of health-related quality of life. The version adapted to Spanish and validated by Alonso, et al. [24,25] was used. The questionnaire allows the calculation of two summary scores, one for Physical Quality Of Life and another for Psy-QoL. The latter has been used as a measure of personal recovery. The authors of the Spanish version reported good psychometric properties in terms of reliability (α>0.75 in all subscales) and validity.
Internalized Stigma of Mental Illness Inventory (ISMI): The IS was measured using the 29-item version of the ISMI. In particular, the version adapted to Spanish and validated by Bengochea-Seco, et al. [26,27] was used. The ISMI items are grouped into five subscales that measure the following dimensions: alienation, stereotype endorsement, discrimination experience, social withdrawal and stigma resistance. The inventory provides a total score that reflects the participant's degree of IS –this was the score used in this study. Bengochea-Seco, et al. [27] reported that their version of the ISMI retains the five-factor structure of the original scale and that it is highly reliable (α=0.91; test-retest=0.95).
Screening for Cognitive Impairment in Psychiatry (SCIP-S): Cognitive functioning, included as a covariate in the mediation analysis, was measured using the SCIP-S test, in its version adapted and validated by Pino, et al. [28,29]. It allows for a rapid assessment of cognitive deficits in a clinical population. The authors of the Spanish version reported adequate psychometric performance on samples of patients with schizophrenia with respect to inter-observer reliability (mean Kappa coefficient=0.99), internal consistency (α=0.73), temporal stability (intraclass correlation coefficient=0.90) and various validity parameters.
Analysis
The presence of childhood trauma as a predictor of poorer personal recovery (Hypothesis 1) was examined through the calculation of partial correlations between the variables included in the study, while controlling for age, haloperidol equivalent dose and cognitive functioning. The level of experiential avoidance and levels of insecure attachment as mediators of the relationship between childhood trauma and personal recovery (Hypotheses 2 and 3), was examined through a simple mediation analysis for each of the dependent variables (IS and Psy- QoL), including as mediators the variables experiential avoidance, anxious attachment, avoidant attachment and, as an independent variable, the frequency of childhood traumas. The variables age, equivalent dose of haloperidol and cognitive functioning were introduced into the model as covariates. The estimation procedure for the simple mediation models was based on the calculation of the 95% confidence intervals through a bias-corrected bootstrapping method (BCI) for 1000 resamples. As a measure of effect size for indirect effects, the proportion mediated (PM) was used [30]. This index represents the proportion that the indirect effects have as mediators over the total effect. The R software was used for statistical analysis [31].
Results
Characteristics of the sample
Table 1 shows the characteristics of the sample and scores of each measure used in the analysis. Descriptive analyses show that 62.4% (n=68) of the participants had experienced at least one traumatic experience in childhood. Of these, 74% (n=50) suffered more than one traumatic experience, with the mean being 3.7 (SD=3).
| Variables | Participants (n=109) | |
|---|---|---|
| Marital status (n; %) | ||
| Single | 98 (89.9) | |
| Married | 4 (3.7) | |
| Separate | 6 (5.5) | |
| Widower | 1 (0.9) | |
| Education (n; %) | ||
| Primary school or below | 50 (45.9) | |
| Secondary school | 31 (28.4) | |
| High school | 19 (17.4) | |
| University or above | 9 (8.3) | |
| Level of education in years (mean; SD) | 11.4 (3.4) | |
| Employment situation (n; %) | ||
| Employee | 2 (1.8) | |
| Unemployed | 107 (98.2) | |
| ExpTra-S (mean; SD) | ||
| Frequency | 3.93 (5.87) | |
| AAQ-II (mean; SD) | 16.83 (9) | |
| PAM (mean; SD) | ||
| Anxious | 0.85 (.51) | |
| Avoidant | 1.28 (.37) | |
| SF-36 (mean; SD) | ||
| Psy-QoL | 45.11 (13.9) | |
| ISMI (mean; SD) | 1.86 (.66) | |
| SCIP-S (mean; SD) | 56.1 (12.51) |
Note: AAQ-II: Acceptance and Action Questionnaire - II; ExpTra-S: Traumatic Experience Screening Questionnaire for Patients with Severe Mental Disorders; ISMI: Internalized Stigma of Mental Illness Inventory; PAM: Psychosis Attachment Measure; SF-36: Short Form Health Survey; SCIP-S: Screening for Cognitive Impairment in Psychiatry.
Correlational analysis
Table 2 shows the results obtained based on the partial correlation analysis [32]. The results indicated positive and significant partial correlations between the dependent variable IS and the independent variable frequency of childhood traumas as well as the mediating variables experiential avoidance and anxious attachment. The dependent variable Psy-QoL showed negative and significant partial correlations with the independent variable frequency of childhood traumas and all mediating variables (Table 2).
| Trauma frequency | Experiential avoidance | Anxious attachment | Avoidant attachment | IS | Psy-QoL | |
| Experiential avoidance | 0.41** | |||||
| Anxious attachment | 0.10 | 0.52* | ||||
| Avoidant attachment | -0.02 | 0.24* | 0.38* | |||
| IS | 0.43** | 0.63* | 0.34* | 0.19 | ||
| Psy-QoL | -0.38** | -0.73* | -0.39* | -0.23* | -0.47* | |
| Mean | 3.93 | 16.83 | 0.85 | 1.28 | 1.86 | 45.11 |
| SD | 5.87 | 9.00 | 0.51 | 0.37 | 1.71 | 13.90 |
Note: *p <0.05; **p <0.01.
Mediational analysis
Table 3 shows the results of the simple mediation models.
| Indirect effects | Direct effects | Overall effects | PM | |||||
|---|---|---|---|---|---|---|---|---|
| Dependent variable | Mediator variable | a | b | a*b | BCI | c’ | c | |
| IS | ||||||||
| AAQ-II | 0.65** | 0.04** | 0.03 | [0.01, 0.04] | 0.02* | 0.05** | 0.53 | |
| PAM-A | 0.01 | 0.38** | 0.01 | [-0.01, 0.01] | 0.04** | 0.05** | 0.08 | |
| PAM-E | <0.01 | 0.36** | <0.01 | [-0.01, 0.01] | 0.05** | 0.05** | <.01 | |
| Psy-QoL | ||||||||
| AAQ-II | 0.65** | -1.06** | -0.69 | [-1.14, -0.30] | -0.23 | -0.92** | 0.75 | |
| PAM-A | 0.01 | -9.46** | -0.09 | [-0.29, 0.04] | -0.82** | -0.92** | 0.1 | |
| PAM-E | <0.01 | -9.13** | -0.01 | [-0.12, 0.10] | -0.92** | -0.92** | <0.01 | |
Note: BCI: Bias-corrected bootstrapping confidence interval; a*b: Indirect effect; a: Regression coefficient of a over b; b: Regression coefficient of b over c; c’: Direct effect; c: total effect; AAQ-II: Experiential avoidance, PAM-A: Anxious attachment; PAM-E: Avoidant attachment; PM: Ratio of the indirect effect to the total effect.
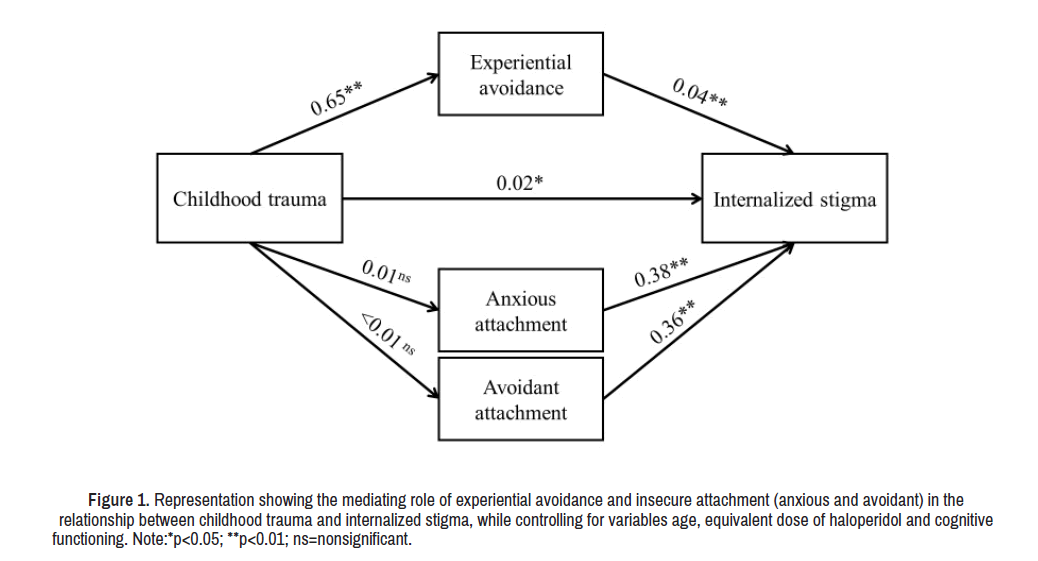
Figure 1 displays the first model of the relationship between childhood trauma and IS with experiential avoidance and insecure attachment as mediators [33]. The model demonstrated that experiential avoidance was the only significant mediator between childhood trauma and IS (a × b=0.03; BCI 95% [0.01, 0.04]). Both the direct effect (c’=0.02; p=0.02; CI 95% [0.01, 0.04]) and the total effect of the model (a × b+c’) were significant (c=0.05; p<0.01; CI 95% [0.03, 0.07]). The analysis of the effect size yielded a PM=0.53, indicating that 53% of the total effect is attributable to the mediated effect [34]. Since childhood trauma did not predict either anxious attachment or avoidant attachment, neither acted as a mediator between childhood trauma and IS (Table 3). Chi-Square goodness of fit test suggested that the model's covariance matrix adequately reproduced the observed data (χ2(3)=4.07, p=0.25). Additional fit indices, such as the approximation mean square error (RMSEA), standardized residual mean square root (SRMR) and comparative fit index (CFI) also met the criteria for a proper model fit: RMSEA=0.05, SRMR=0.04, CFI=0.98.
Figure 1. Representation showing the mediating role of experiential avoidance and insecure attachment (anxious and avoidant) in the relationship between childhood trauma and internalized stigma, while controlling for variables age, equivalent dose of haloperidol and cognitive functioning. Note:*p<0.05; **p<0.01; ns=nonsignificant.
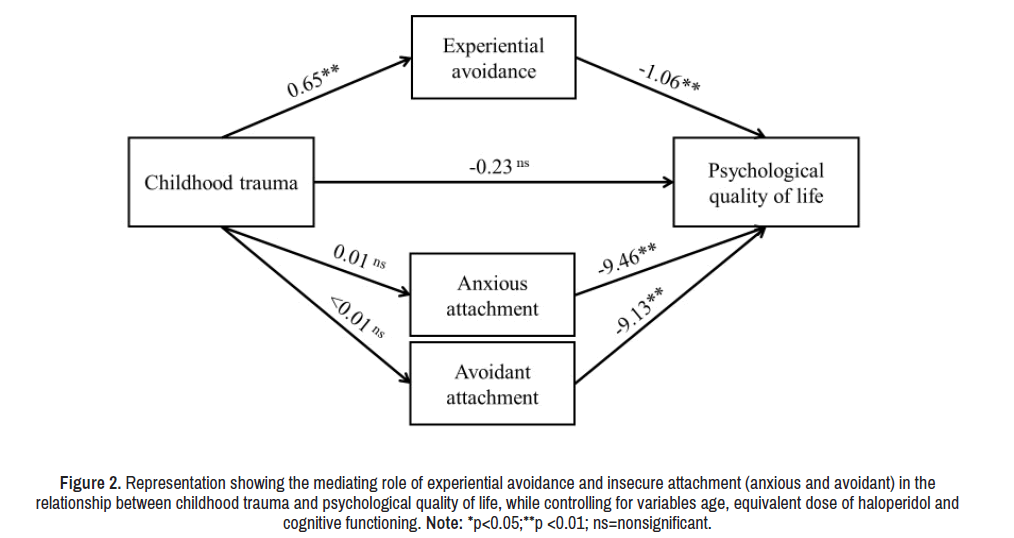
Figure 2 displays the model of the relationship between childhood trauma and Psy-QoL with experiential avoidance and insecure attachment as mediators [35]. In this model, as in the previous one, experiential avoidance was the only mediating variable between childhood trauma and Psy-QoL (a × b= -0.69; BCI 95% [-1.14,-0.30]) with non-significant direct effects (c’= -0. 23; p=0.27; CI 95% [-0.69, 0.22]), [36] significant total effects (c=0.92; p<0.01; CI 95% [-1.29, -0.50]) and a PM effect size=0.75– this indicates a percentage of the mediated effect of 75%. Given the lack of prediction of childhood trauma on anxious attachment and avoidant attachment, neither acted as mediators between childhood trauma and IS (Table 3).[37] Regarding the fitting of this mediated model, the proposed indices showed adequate values (χ2(3)=4.07, p=0.25; RMSEA=0.05; SRMR=0.04; CFI=0.97).
Figure 2. Representation showing the mediating role of experiential avoidance and insecure attachment (anxious and avoidant) in the relationship between childhood trauma and psychological quality of life, while controlling for variables age, equivalent dose of haloperidol and cognitive functioning. Note: *p<0.05;**p <0.01; ns=nonsignificant.
Discussion and Conclusion
Partial correlation analysis confirmed the first hypothesis, according to which childhood trauma is associated with poorer personal recovery in patients with schizophrenia. The results show that the presence of childhood trauma is significantly related to higher levels of IS and worse Psy-QoL, even after controlling for the effects of age, equivalent dose of haloperidol and level of cognitive functioning. These results are consistent with those obtained by Outcalt and Lysaker who reported a relationship between a history of trauma and an increased level of IS in patients with schizophrenia. Our findings also expand on previous research that reported a relationship between a history of childhood trauma and poorer clinical recovery, by noting that such experiences also impact on personal recovery.
Meanwhile, experiential avoidance showed a negative influence on personal recovery, being associated with a higher level of IS and lower Psy- QoL scores. These results are consistent with those obtained by previous research in which it was found to be associated with poorer recovery in people with schizophrenia, both in clinical terms and in personal terms. However, the results of the present study go further by finding that experiential avoidance plays a mediating role between childhood trauma and personal recovery, thus confirming our second hypothesis. Specifically, experiential avoidance partially mediates the relationship between childhood trauma and the level of IS –explaining 53% of this relationship– and fully mediates the relationship between childhood trauma and the level of Psy-QoL – explaining 75% of this relationship. This finding supports the hypotheses derived from Garety and Freeman's cognitive model of psychosis according to which the use of maladaptive emotional regulation strategies in people with schizophrenia would lead to cognitive biases and misinterpretation of their own negative affective states, negatively impacting their clinical and personal recovery.
In line with expectations, our results show that insecure attachment also predicts worse personal recovery. This extends the results of previous research such as the meta-analysis by Carr, et al. in which, after analyzing 25 quantitative studies (n=11.696), a significant relationship was found between insecure attachment and greater severity of positive symptoms (an indicator of poor clinical recovery). However, in the present study – in contrast to the findings of other research – childhood trauma showed no relationship with insecure attachment as measured by the PAM, which disconfirms our third hypothesis. A plausible explanation for this finding is that the ExpTra-S scale measures a wide variety of childhood traumatic events while insecure attachment has been linked to a specific class of childhood traumas: those that come from significant others in the child's environment (e.g. primary caregivers) In addition, the PAM does not measure the level of disorganized attachment, which has been consistently linked to childhood trauma as well as to schizophrenia spectrum disorders. The potential influence of disorganized attachment as an explanatory mechanism should be tested in future research.
It should be noted that the generalization of these results should be made with caution given the limitations of the present study. The most important of these limitations has to do with the sample, which was selected based on availability and composed of chronic patients, mostly male. Furthermore, the study does not allow the establishment of causal relationships, something that should be addressed in future research through prospective and longitudinal designs. We also believe that in future, protective factors against the negative impact of childhood trauma should be explored, which would expand the range of potential therapeutic targets.
The above highlights that people with schizophrenia who have a history of childhood trauma and high levels of experiential avoidance constitute a population that requires special clinical attention including traumasensitive interventions aimed at promoting their personal recovery. In this regard there are trauma-focused interventions, such as Trauma-Focused Cognitive Behavior Therapy (TF-CBT), which have revealed promising evidence when used to treat people with schizophrenia. Mindfulness-based interventions may also be relevant for this population since they have proven to be effective in addressing schizophrenia, especially as one of their mechanisms of action is the development of acceptance as a psychological process working against the effects of experiential avoidance.
References
- Vita, Antonio and Stefano Barlati. “Recovery from Schizophrenia: Is it Possible?” Curr Opin Psychiatry31 (2018): 246-255.
- Deegan, Patricia E. "Recovery: The Lived Experience of Rehabilitation."Psychosocial Rehabilitation Journal 11 (1988): 11.
- Lemos-Giráldez, Serafín, Leticia García-Alvarez, Mercedes Paino and Eduardo Fonseca-Pedrero, et al. “Measuring Stages of Recovery from Psychosis.”Compr Psychiatry 56 (2015): 51-58.
- Penas,Patricia, Ioseba Iraurgi,M Concepción Moreno and Jose J Uriarte. “How is Evaluated Mental Health Recovery?: A Systematic Review.”Actas Esp Psiquiatr 47 (2019): 23-32.
- Chiu, Marcus YL, Winnie WN Ho, William TL Lo and Michael GC Yiu. “Operationalization of the SAMHSA Model of Recovery: A Quality of Life Perspective.”Quality Life Res19 (2010): 1-13.
- Pyle, Melissa, Stephen Pilling, Karen Machin and Ginny Allende-Cullen, et al. “Peer Support for Internalised Stigma Experienced by People with Psychosis: Rationale and Recommendations.”Psychosis10 (2018): 146-152.
- Mørkved, Nina, Dagfinn Winje, Anders Dovran and Kjersti Arefjord, et al. “Childhood Trauma in Schizophrenia Spectrum Disorders as Compared to Substance Abuse Disorders.” Psychiatry Res261 (2018): 481- 487.
- Trotta, A, RM Murray and HL Fisher. “The Impact of Childhood Adversity on the Persistence of Psychotic Symptoms: A Systematic Review and Meta-Analysis.”Psychol Med45 (2015): 2481-2498.
- Ludwig, Lea, Dirk Werner and Tania M Lincoln. “The Relevance of Cognitive Emotion Regulation to Psychotic Symptoms:A Systematic Review and Meta-Analysis.”Clin Psychol Rev 72 (2019): 101746.
- Hayes, Steven C, Kelly G Wilson, Elizabeth V Gifford and Victoria M Follette, et al. “Experiential Avoidance and Behavioral Disorders: A Functional Dimensional Approach to Diagnosis and Treatment.”J Consult Clin Psychol64 (1996): 1152-1168.
- O'Driscoll, Ciarán, Jennifer Laing and Oliver Mason. “Cognitive Emotion Regulation Strategies, Alexithymia and Dissociation in Schizophrenia: A Review and Meta-Analysis.”Clil Psychol Rev34 (2014): 482-495.
- Grezellschak, Sarah, Andreas Jansen and Stefan Westermann. “Emotion Regulation in Patients with Psychosis: A Link Between Insomnia and Paranoid Ideation?”J Behav Ther Exp Psychiatry 56(2017): 27-32.
- Valiente, Carmen, Maria Provencio, Regina Espinosa and Almudena Duque, et al. “Insight in Paranoia: The Role of Experiential Avoidance and Internalized Stigma.”Schizophr Res164 (2015): 214-220.
- Gratz, Kim L, Marina A Bornovalova, Ayesha Delany-Brumsey and Bettina Nick, et al. “A Laboratory-Based Study of the Relationship Between Childhood Abuse and Experiential Avoidance Among Inner-City Substance Users: The Role of Emotional Nonacceptance.”Behav Ther38 (2007): 256-268.
- Carr, Sarah Christina, Amy Hardy and Miriam Fornells-Ambrojo. “Relationship Between Attachment Style and Symptom Severity Across the Psychosis Spectrum: A Meta-Analysis.” Clin Psychol Rev 59 (2018): 145-158.
- Gumley, AI, HEF Taylor, M Schwannauer and A MacBeth. “A Systematic Review of Attachment and Psychosis: Measurement, Construct Validity and Outcomes.”Acta Psychiatr Scand 129 (2014): 257-274.
- Vasileva, Mira and Franz Petermann. “Attachment, Development, and Mental Health in Abused and Neglected Preschool Children in Foster Care: A Meta-Analysis.”Trauma Violence Abuse19 (2018): 443-458.
- Leucht, Stefan, Myrto Samara, Stephan Heres and Maxine X Patel, et al. “Dose Equivalents for Second-Generation Antipsychotic Drugs: The Classical Mean Dose Method.”Schizophr Bull41 (2015): 1397-1402.
- Ordóñez Camblor, Nuria, Eduardo Fonseca Pedrero, María de las Mercedes Paíno Piñeiro and Leticia García Álvarez, et al. “Evaluation of Early Traumatic Experiences In Adults.” Roles of the Psychologist 37 (2016) 36-44.
- Bond, Frank W, Steven C Hayes, Ruth A Baer, and Kenneth M Carpenter, et al. “Preliminary Psychometric Properties of the Acceptance and Action Questionnaire–II: A Revised Measure of Psychological Inflexibility and Experiential Avoidance.”Behav Ther42 (2011): 676-688.
- Ruiz, Francisco J, Alvaro I Langer Herrera, Carmen Luciano and Adolfo J Cangas, et al. “Measuring Experiential Avoidance and Psychological Inflexibility: Spanish Version of the Acceptance and Action Questionnaire-II.” Psicothema 25 (2013): 123-129.
- Berry, Katherine, Alison Wearden, Christine Barrowclough and Tom Liversidge. “Attachment Styles, Interpersonal Relationships and Psychotic Phenomena in a Non-Clinical Student Sample.”Pers Individ Differ 41 (2006): 707-718.
- Sheinbaum, Tamara, Katherine Berry and Neus Barrantes-Vidal. “Spanish Version of the Psychosis Attachment Measure: Adaptation Process and Psychometric Properties.”Salud ment36 (2013): 403-409.
- Ware Jr, John E and Cathy Donald Sherbourne. “The MOS 36-Item Short-Form Health Survey (SF-36): I. Conceptual Framework and Item Selection.”Med Care(1992): 473-483.
- Alonso, J, L Prieto and J M Anto. “The Spanish Version of the SF-36 Health Survey (the SF-36 Health Questionnaire): an Instrument for Measuring Clinical Results.”Med Clín 104(1995): 771-776.
- Ritsher, Jennifer Boyd, Poorni G Otilingam and Monica Grajales. “Internalized Stigma of Mental Illness: Psychometric Properties of a New Measure.”Psychiatry Res121 (2003): 31-49.
- Bengochea,Seco, Rosario, Marta Arrieta-Rodríguez and Mar Fernández-Modamio, et al. "Adaptation into Spanish of the Internalised Stigma of Mental Illness Scale to Assess Personal Stigma."Rev Psiquiat Salud Ment 11 (2018): 244-254.
- Purdon, S and R Psych. "The Screen for Cognitive Impairment in Psychiatry:Administration and psychometric properties.” Edmonton Alberta Canada: PNL(2005).
- Pino O, Guilera G, Rojo JE, Gómez-Benito and J, Purdon SE. “SCIP-S, Screening Del Deterioro Cognitivo en Psiquiatría.” Madrid: Tea Ediciones (2014).
- Fairchild, Amanda J and Heather L McDaniel. “Best (but Oft-Forgotten) Practices: Mediation Analysis.”Am J Clin Nutr105 (2017): 1259-1271.
- RDC Team. “R: A Language and Environment for Statistical Computing.” Vienna: R Foundation for Statistical Computing (2006).
- Outcalt, Samantha D and Paul H Lysaker. “The Relationships Between Trauma History, Trait Anger, and Stigma in Persons Diagnosed with Schizophrenia Spectrum Disorders.”Psychosis4 (2012): 32-41.
- Garety, PA and D Freeman. "The Past and Future of Delusions Research: From the Inexplicable to the Treatable."Br J Psychiatry203 (2013): 327-333.
- Rholes, W Steven, Ramona L Paetzold and Jamie L Kohn. “Disorganized attachment mediates the link from early trauma to externalizing behavior in adult relationships.”Personality Individual Differences90 (2016): 61-65.
- Steel, Craig, Amy Hardy, Ben Smith and Til Wykes, et al. “Cognitive–Behaviour Therapy for Post-Traumatic Stress in Schizophrenia: A Randomized Controlled Trial.”Psychol Med47 (2017): 43-51.
- Swan, Sarah, Nadine Keen, Nicola Reynolds and Juliana Onwumere. “Psychological Interventions for Post-Traumatic Stress Symptoms in Psychosis: A Systematic Review of Outcomes.”Front Psychol 8 (2017): 341
- Hodann-Caudevilla, Ricardo M, Cintia Díaz-Silveira, Francisco A Burgos-Julián and Miguel A Santed. “Mindfulness-Based Interventions for People with Schizophrenia: A Systematic Review and Meta-Analysis.”Int J Environ Res Public Health17(2020): 4690.
Citation: Hodann-Caudevilla, Ricardo M, Juan Jesús Muñoz García and Francisco Alfonso Burgos Julián. "Childhood Trauma and Personal Recovery in Schizophrenia: Mediating Role of Experiential Avoidance and Insecure Attachment.” Clin Schizophr Relat Psychoses 15(2021) Doi: 10.3371/CSRP.RMGJ.070421.
Copyright: © Ricardo MHC, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.